4 Mental Health and Substance Use
Introduction
Mental health and substance abuse are both multifaceted, challenging, and dynamic areas of the human service field. As professionals in this field, social workers help to make long lasting, life altering changes in people’s lives.
While numerous books have been written about mental disorders and substance use both broadly and specifically, this chapter will seek to introduce you to current information about mental disorders and substance use in the United States. This chapter will include, among other things, a brief history of both mental health and substance use, the current terminologies and definitions that professionals use in the field, some of the most commonly occurring disorders and/or substances that a social worker is likely to encounter in general practice, and briefly discuss the co-occurrence of mental disorders and substance use.
Vincent Van Gogh (self-portrait: Above) may have suffered from numerous conditions including bipolar disorder or manic-depressive disorder (Wolf, 2001). He is an example of how mental disorders and creativity can go hand in hand and how people living with a mental disorder can still be productive members of society.
Before We Get Started
Before we begin, it is important to understand some of the keywords, definitions, and sources that will be used. These are a small sample of the vast vocabulary that is used to identify and describe the mental disorders and substance use disorders that social workers may encounter in professional settings.
Key Terms
- Behavior – the response of an individual, group, or species to its environment
- Co-occurring – to appear together in sequence or simultaneously.
- Delusion – a false belief or opinion.
- Dual Diagnosis – when a person has two separate illnesses and each illness needs a treatment plan (DBSA, 2016).
- Hallucination – a sensory experience of something that does not exist outside the mind, caused by various physical and mental disorders, or by reaction to certain toxic substances, and usually manifested as visual or auditory images.
- Inpatient – a patient who stays in a hospital while receiving medical care or treatment.
- Mania – excessive excitement or enthusiasm; craze.
- Manic – pertaining to or affected by mania.
- Mental Disorder – any of the various forms of psychosis or severe neurosis.
- Outpatient – a patient who receives treatment at a hospital, as in an emergency room or clinic, but is not hospitalized.
- Prevalence – being widespread; of in wide extent or occurrence.
- Psychosis – a mental disorder characterized by symptoms, such as delusions or hallucinations, that indicate impaired contact with reality.
Definitions retrieved via Dictionary.com (2017), unless otherwise noted.
Mental Health
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (2013), also known as the DSM-5, is a living document created by social workers, psychologists, medical doctors and many other professions. The DSM-5 is the primary reference source social workers and other helping professions use to describe a mental disorder. In this text, just as in the DSM-5, “mental disorder” will be used as a broad term to describe several issues related to emotion, mental state, and behavior. However, this text is not enough to help people with a mental disorder. It takes a generalist approach from social workers, as well as other health professionals, to not just identify the disorder but then advocate on behalf of that person, provide supportive services, and work with the many challenges that accompany mental health disorders. Being a generalist means that the social worker employs various methods of treatment, expertise and skills to assist the client. Examples of methods used might be a strengths based approach where the client is encouraged to focus on and use their inherent strengths (not just physical ones) to improve other areas of their life. Social workers also focus on the person in environment. This means that social workers are aware of the impact the person has on their environment and how the environment impacts the person.
According to the National Alliance on Mental Illness (NAMI), approximately 1 in 5 adults in the United States experience some type of mental disorder in a given year. This means that, in a population of over 325 million people, over 43 million people will experience some form of mental health issue within a year. Among those that do experience a mental disorder, 9.8 million of those will experience a “severe” mental disorder meaning that it dramatically interferes or limits their ability to function in their everyday life. Of all the adults in the United States with a mental disorder, only 41% received mental health services in the past year. For those with a severe disorder, only 63% received any form of treatment or services (NAMI, 2017). Looking at those numbers it is clear to see that the need to identify, de-stigmatize and help individuals living with mental disorders, will impact millions of people.
There are six categories of mental disorders that this chapter will focus on as well as the variety of disorders found within those categories. These categories contain some of the most common disorders that a social worker will encounter in her or his career. This chapter also provides a brief description of the disorders as well as the estimated occurrence, or prevalence, of each one within the United States.
The selected categories are:
- Anxiety Disorders
- Psychotic Disorders
- Bipolar Disorders
- Depressive Disorders
- Trauma Disorders
- Personality Disorders.
History of Mental Health
Historically, people suffering from a mental disorder have also suffered abuse, experimentation, torture, and even death. As you go forth as a member of the social work profession, it is imperative that you understand how long of a road it has been and how much further the profession needs to go in the ethical treatment of people with a mental disorder. This link to a 27-minute video provides an example of where we were at just a few decades ago. The Willowbrook State School in New York City is one example of a tragic and possibly disturbing look the past treatment of those with a mental disorder and the developmentally disabled.
As you can see from the video, the Willowbrook Institute lacked funding, professionals, and knowledge of what their patients needed to be able to live successfully. Unfortunately, the Willowbrook Institute was not an isolated incident, nor was it a new occurrence. Historically, those with a mental disorder have been looked down upon, shunned, stigmatized, vilified, criminalized or tortured. This kind of treatment has been documented as far back as the middle ages of Europe all the way to the mid 1900’s- United States where those with a mental disorder were placed in either hospitals or prisons.
This treatment continued up until 1963 when John F. Kennedy signed the Community Mental Health Act. President Kennedy described it as “a bold new approach”, and provided federal grants to states to construct community mental health centers (CMHC), to improve the delivery of mental health services, preventions, diagnosis, and treatment to individuals who reside in the community. To be able to supply federal funding for these statewide institutions, the Medicaid Act was passed in 1965. This Act allowed community-based care facilities to charge for reimbursement of funds while excluding payments to psychiatric institutions.

The Community Mental Health Act resulted in a mass “deinstitutionalization” across the country, and by 1980 nearly 75% of the psychiatric hospital population had declined. By 2009 less than 2% of those suffering from a mental health disorder remained in institutions. Unfortunately, this resulted in some unintended consequences. For example, community-based institutions could not keep up with the mass exodus of people from the psychiatric hospitals. This was the result of several factors such as a lack of space within the inpatient and outpatient settings, a lack of funding for proper care, and a lack of funding to improve care facilities. This lack of resources has negatively impacted the care and treatment of adults, children, families, and communities across the country.
Things to Be Aware Of
Having a mental disorder is often compared to having a physical illness (APA, 2015) and the comparison is one that professionals can often overlook. Just as there are varying degrees of physical illnesses, there are also varying degrees of mental disorders. The mental disorders can be managed in similar ways to physical ones. By maintaining medications, therapy, and problem-solving with the individual, social workers can help the person to not only stabilize, but excel in, their life. In fact, there are many successful individuals both in today’s world and throughout history, such as Vincent Van Gogh, who have found ways to cope with their mental disorders. Van Gogh most likely had one, maybe even two, mental disorders. Despite, or maybe because of, these challenges he was able to produce some of the most iconic and famous pieces of modern art to this date.
Being aware of the following mental disorders will allow you, as a social worker to better understand what the person is experiencing and how to help them meet their needs in the best possible way.
While every case is different, it is important to start thinking about some of the ways that mental disorders may present themselves. To assist you in this task some brief case studies have been provided throughout the chapter. These case studies are based on the experiences and case notes of real people and professionals.
All information and statistics following are from the DSM-5 unless otherwise indicated.
Anxiety Disorders:
Anxiety disorders are characterized by shared features like excessive fear (the emotional response to real or perceived imminent threat) and anxiety (anticipation of future threat) and other related behavioral disturbances.
● Social Anxiety Disorder or “Social Phobia” is an extreme fear of being judged by others in social situations. The fear is so intense that it will disrupt or impair the person’s ability to function in their everyday life. There is about a 7% prevalence in the United States for this disorder.
● Generalized Anxiety Disorder is an excessive, often unfounded, feeling of worry about the numerous everyday activities that a person could engage in. Approximately 2.9% of adults in the United States report symptoms or seek treatment for this disorder.
● Phobias are, simply put, an irrational fear of something. You may have heard of arachnophobia (fear of spiders) or acrophobia (fear of heights). In the United States, approximately 7%-9% of the population reports having a specific phobia and around 75% of this population will fear more than one object.
● Panic Disorder is defined as a debilitating fear or anxiety that occurs without any reasonable explanation. It is estimated that 2%-3% of the United States adult population will experience an episode of panic disorder in a year.
Case Sudy: Kristen
Kristen is a 38-year-old divorced mother of two teenagers. She has had a successful, well-paying career for the past several years in upper-level management. Even though she has worked for the same company for over 6 years, she’s found herself worrying constantly about losing her job and being unable to provide for her children. This worry has been troubling her for the past 8 months. Despite her best efforts, she hasn’t been able to shake the negative thoughts.
Kristen has found herself feeling restless, tired, and tense. She often paces in her office when alone. When she goes to bed at night, it’s as if her brain won’t shut off. She finds herself mentally rehearsing all the worse-case scenarios regarding losing her job, including ending up homeless (Case Studies, 2015).
What do you think Kristen might be diagnosed with?
Psychotic Disorders:
Psychotic disorders among the most serious and challenging disorders. This is because these disorders affect an individual’s interpretation of reality which then negatively impacts the person’s ability to function in their environments. Across the spectrum of psychotic disorders there are common symptoms such as hallucinations, delusions, or behaviors that are considered socially abnormal.
● Schizophrenia is a chronic and severe mental disorder that affects how a person thinks, feels, and behaves (NAMI, 2016). These disturbances may present as hallucinations or delusions. Adults in the United States report a lifetime prevalence of 0.3%-0.7%, with an age of onset often occurring in the early to mid-20s.
● Delusional Disorder is the presence of one or more delusions. These delusions must be present for at least one month to the DSM-5 definition for this disorder. The prevalence of this disorder occurs in 0.2% of adults in the United States.
● Schizoaffective Disorder is characterized by schizophrenic symptoms, such as delusions or hallucinations, but with an added component of a mood disorder like mania and depression. About 0.3% of the United States adult population with be diagnosed with schizoaffective disorder in a year (NAMI, n.d.).
Case Study: Martin
Martin is a 21-year-old business major at a large university. Over the past few weeks his family and friends have overheard him whispering in an agitated voice even though there is no one nearby. Lately, he has refused to answer or make calls on his cell phone, claiming that if he does it will activate a deadly chip that was implanted in his brain by evil aliens.
His parents have tried to get him to go to a psychiatrist for an evaluation, but he refuses. He has accused them of conspiring with the aliens to have him killed so they can remove his brain and put it inside one of their own. He has stopped attended classes altogether. He is now so far behind in his coursework that he will fail if something doesn’t change very soon (Case Studies, 2015).
What do you think Martin could be diagnosed with?
Bipolar Disorders:
A bipolar disorder can be defined as a variance in brain functioning that can cause unusual shifts in mood, energy, or activity levels. These shifts interfere with the person’s ability to carry out day-to-day tasks. These disorders can display a range of heightened emotions in the form of manic episodes (extreme ups) to depressive episodes (extreme downs) (NAMI, 2016).
● Bipolar Disorder I is a period of mania presented as persistently elevated, irritable mood, and persistently increased activity accompanied by feelings of euphoria (being excessively cheerful) or feeling “on top of the world.” The prevalence of adults in the United States with this disorder is 0.6%.
● Bipolar Disorder II is a milder form of mood elevation, involving mild episodes of mania, where one feels hyperactive and elated, that alternate with periods of severe depression, feeling down or sad for no obvious reason. Across a one-year span in the United States, about 0.8% of adults will meet criteria for this disorder.
Depressive Disorders:
Depression affects an estimated 300 million people globally and more than 15 million adults (6.7% of the population) in the United States. There are several levels of depression as well as minor levels that co-occur with other disorders or that are brought on by substance use/withdrawal.
● Major Depressive Disorder is a period of low mood for at least two weeks that is present most of the time in most situations. This may look like low self-esteem, low energy, or loss of enjoyment in pleasurable activities. Major depressive disorder will affect about 6.7% of the adult population in the United States (Facts and Statistics, 2016)
● Persistent Depressive Disorder, while lacking the severity of major depression, is a chronic, or ongoing, period of depression, usually for at least two years. Approximately 1.5% of the adult population of the United States will qualify under its criteria (ADAA, 2016)
Case Study: Jessica
Jessica is a 28-year-old married female. She has struggled with significant feelings of worthlessness and shame due to her inability to perform as well as she always has in the past. Jessica has found it increasingly difficult to concentrate at work. Jessica’s husband has noticed that she has called in sick on several occasions. On those days, she stays in bed all day, watching TV or sleeping. He’s overheard her having frequent tearful phone conversations with her closest friend which have him worried. When he tries to get her to open up about it, she pushes him away with an abrupt “everything’s fine.”
Although she hasn’t ever considered suicide, Jessica has found herself increasingly dissatisfied with her life. She’s been having frequent thoughts of wishing she was dead. She feels like she has every reason to be happy, yet can’t seem to shake the sense of doom and gloom that has been clouding each day as of late.
What do you think Jessica might be diagnosed with?
Trauma Disorders:
● Post-traumatic Stress Disorder (PTSD) can be brought on after experiencing, witnessing, or hearing about a traumatic event. This is most often associated with military personnel/veterans or victims of war. However, traumatic events can be shootings, physical assaults, or rape. After a month of being removed from the event a person may experience sleeplessness, increased heart rate, mood shifts, physically lashing out, or any combination of responses. These changes may be brought on by any stimulus in the environment that reminds the person of the terrifying event or from experiencing recurring thoughts about the event. In the United States, about 3.5% of adults will report experiencing some form of PTSD within a given year.
● Acute Stress Disorder can be described as the symptoms of post-traumatic stress disorder lasting for three days to one month. If it lasts for longer than one month, it than meets the criteria for PTSD. Acute Stress Disorder is reported in less than 20% of non-assault related events; it is reported in 20%-50% from related events like rape, assault, or witnessing a mass shooting.
Case Study: Josh
Josh is a 27-year-old male whose fiancée of four years was killed by a drunk driver 3 months ago. She died in his arms in the middle of the crosswalk. No matter how hard he tries to forget, he frequently finds himself reliving the entire incident.
He had to quit his job because his office was located in the building right next to the place of the incident. The few times that he attempted to return to work were unbearable for him. He has since avoided that entire area of town.
Normally an outgoing, fun-loving guy, Josh has become increasingly withdrawn, “jumpy”, and irritable. He’s stopped working out, playing his guitar, or playing basketball, all activities he once really enjoyed. His parents worry about how detached and emotionally flat he’s become.
(DeepDiveAdmin, 2015)
What do you think Josh might be diagnosed with?
Personality Disorders:
A personality disorder is a pattern of inner experiences and behavior that deviates from the expectations of the individual’s culture, is continuous, enduring and inflexible; it often has an onset in adolescence or early adulthood and leads to distress or impairment in the person’s life.
These types of personality disorders are often experienced by people seeking community mental health treatment and the homeless population, both areas social workers are employed. Some personality disorders that you might encounter include:
● Paranoid personality disorder which is a pattern of distrust and suspicion of others’ motives. These motives may be interpreted as malevolent or harmful to the person experiencing the paranoia. Paranoid personality disorder may be as prevalent as 4.4% among adults in the United States.
● Schizoid personality disorder is a pattern of detachment from social relationships and a restricted range of emotional expression. The prevalence of this disorder ranges from 3.1%-4.9% of the United States adult population.
● Antisocial personality disorder is a pattern of disregard for, and violation of, the rights of others. Those who display the symptoms of this disorder may habitually lie, commit aggressive or violent acts with little to no remorse, and violate social norms. The prevalence of this disorder ranges from 0.2%-3.3%.
● Borderline personality disorder is a pattern of instability in interpersonal relationships, self-image, and affect. People with borderline personality disorder may be overly impulsive or not understand social norms. It is estimated that 1.6% to as much as 5.9% of the United States adult population will be diagnosed with this disorder.
● Narcissistic personality disorder is a pattern of grandiosity, need for admiration, and lack of empathy. 6.2% of the adult population will report for this disorder within a year.
● Obsessive-compulsive personality disorder is a pattern of preoccupation with orderliness, perfectionism, and control. This preoccupation may impair their social lives, health, or ability to function in the outside environment. The prevalence for this disorder ranges from 2.7%-7.9% in a one-year period among the adult population in the United States.
Practice Settings
There are two main practice settings where you as the social worker are likely to encounter people with mental disorders: inpatient (hospitals, medical & psychiatric) and outpatient (mental health clinics). Though there are some similarities in goals and strategies, the differences are certainly worth noting.
Inpatient services in these settings are provided by social workers who work with individuals or groups to provide treatment in a variety of forms. The inpatient worker also works with friends, family, and employers to help the person return to their outside life. The social worker may advocate and work with other agencies to provide assistance or resources for individuals under their purview of care.
When a patient is ready to leave a psychiatric facility, the social worker may connect them to an outpatient clinic. In these settings, outpatient workers assist the individuals or groups in maintaining healthy functioning in their environment through therapy or clinical activities. The social worker in this setting will conduct therapy or planning sessions, contact outside agencies, and advocate for their client’s best interests.
Vulnerable Populations
While many people living with a mental disorder live fulfilling lives those who have a “severe” mental disorder are considered a vulnerable population. When we refer to people or a population as vulnerable this means it is “the degree to which a population, individual or organization is unable to anticipate, cope with, resist and recover from the impacts of disasters” (WHO, 2017). This vast population overlaps with several other populations that will/have been covered in this book:
● Veterans
● Children
● Poor/Disenfranchised
● LGBTQ+
● Minorities
● Homeless
● Prisoners
● Seniors
Things to Be Aware Of
The field of mental health is not perfect. Studies can only give us so much insight into the symptoms, behaviors, predictors, prevalence and other criteria used in identifying mental disorders. The DSM-5, while a useful tool, is still scrutinized for numerous reasons. For instance, this is the fifth edition of this text meaning that things have changed in definitions and classifications across the decades. The DSM-5, unlike its four previous versions, is being treated as a “living document” and will be amended more frequently in coming years than its previous versions. With this idea of a “living document” in mind, it is important to ask some questions. Is the DSM-5 a tool that attaches “labels” to people, thereby inhibiting the treatment that they seek? Is it a tool used only for insurance purposes? Does the collaboration between various backgrounds help or hurt the cause for proper mental health care? There are many more questions, critiques, and changes surrounding, not just the DSM-5, but therapy styles as well as our ever-improving understanding of the brain and we in the social work profession must be aware of them.
These changes have resulted in improvements to how we approach the concept of “mental disorders” as well as adhere more closely to the social worker core values and perspectives. For example, homosexuality used to be classified as a mental disorder but now we know that is simply not the case. Gender dysphoria is now more closely understood as the anxiety experienced due to the pressures of social norms rather than an internal struggle. There are many other changes, both big and small, between the DSM-IV and DSM-5 that are highlighted here.
But it’s not enough to just be aware of what we do in clinical settings. We also must be cognizant of our understanding of trauma (in its many forms), of a client’s resources and of society’s perception of what a mental disorder is. These things will continue to morph throughout time so it is important to remain vigilant and flexible regarding the many changes that occur in our field.
Current Issues
At the time of this book’s publication in late 2017, there are several pieces of legislation that could have important impacts on the services that social workers and other helping professionals offer. For example, the result of the debate over our national healthcare will have a profound impact on who receives Medicaid, how much the states will receive to supplement the costs of Medicaid funding, and what types of services will be covered. In the State of Michigan, for example, the legislators are looking to implement a bill that would take funding from direct providers like Community Mental Health and direct it towards private organizations. This link gives further description of this bill and will allow you, the reader, to form your own opinions http://www.michigan.gov/mdhhs/0,5885,7-339-71550_2941_76181—,00.html
Regardless of what your decisions or thoughts are on these issues are, the social work profession must always be vigilant to who/what/where/why/when of funding. We must also be aware politically of who’s in charge, what their agenda is, and if it impacts our profession, impacts the people we serve, and if it is in line with our professional ethics.
Substance Abuse/Use/Dependence
For decades, a war has raged across the globe. The financial costs have been high, the lives impacted even higher. During this time, we have been told to “Just Say No” and many have been arrested and imprisoned for participating in this war. The enemy in this war has taken many forms and continues to persist in modern times. It is not terror and it is not a tyrannical government. This is a war against drugs.
History of Substance Use
Discussing substance use/abuse would be incomplete without mentioning the “war on drugs” and the historical impact substances/drugs have had on our economy, population, education, law enforcement, and policy.
Made popular in 1971, President Richard Nixon declared drug abuse “public enemy number one.” This statement came along with a dedication of more federal resources towards “prevention of new addicts and the rehabilitation of those who are addicted.” This was not a new idea by any means. The drug war may have started as early as 1860 from certain laws at local levels. After that came the first federal law, the Harrison Narcotics Tax Act, which was signed into law in 1914. Then came Prohibition that, though ultimately unsuccessfully in its attempt to make alcohol illegal, was still an attempt at eliminating an object of public consumption (Thirty Years of America’s Drug War a Chronology, 2014).
This is just the tip of the iceberg as far as the historical legislation of the war on drugs. But the question we should ask is: Are these policies and means of “combating drugs” really working?
According to The National Center on Addiction and Substance Abuse (2017), over $51 billion dollars is spent annually in the United States to combat illegal drugs and their use. For every dollar spent however, only two cents goes towards prevention and treatment of those seeking assistance from a substance use disorder. The rest of the money goes towards prosecution, imprisonment, and hospital costs.
These policies have also lead to an increase the incarceration of individuals, many of whom are in jail or prison for possession, not selling or distribution (Bureau of Justice Statistics, 2007).
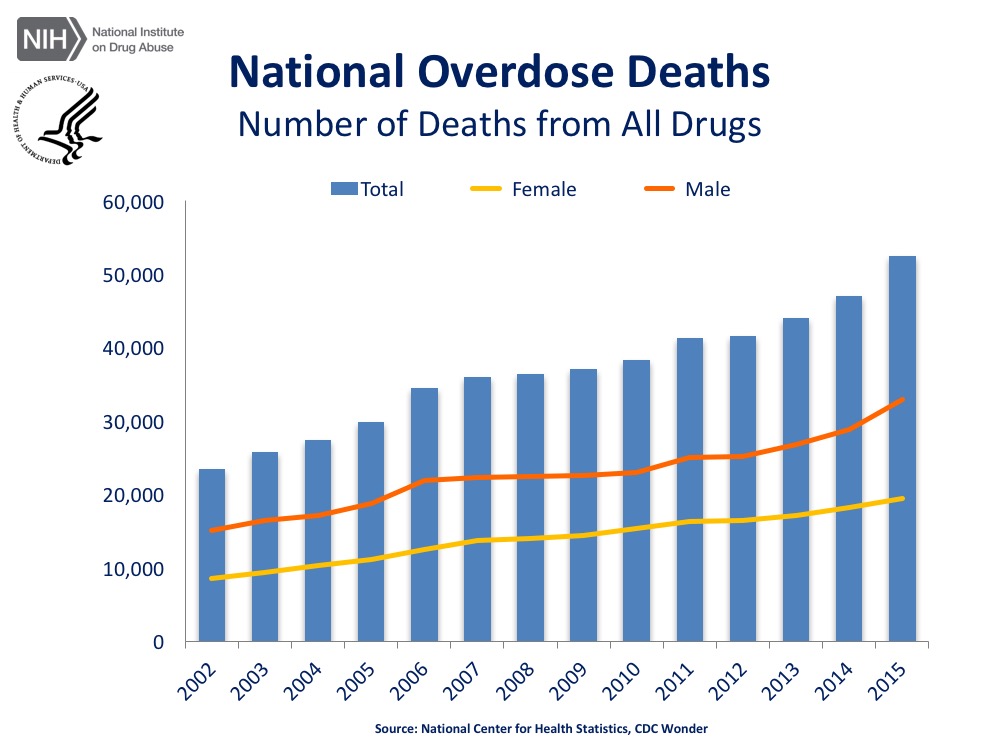
And yet it has not helped address number of deaths from drug use.
To be clear, this is not to say that there should not be drug laws. Rather, the suggestion here is to consider that maybe these laws and investments are causing more harm to the victims of drug use. Perhaps these laws are not designed to prevent their use or help users to rehabilitate, as Nixon originally intended all those years ago?
The World Health Organization (WHO) states:
“Policies which influence the levels and patterns of substance use and related harm can significantly reduce the public health problems attributable to substance use, and interventions at the health care system level can work towards the restoration of health in affected individuals.” (WHO, 2017)
Things to Be Aware Of
It is important to note that the DSM-5 does not use the term “addiction” as a classification term. Some in the helping professions believe the term “addiction” can carry a negative connotation and is a very ambiguous definition. Therefore, the phrase “substance use disorder” is used as a more neutral term by these professionals for the purposes of describing the variety of ways that this disorder can be identified.
Key Terms
- Abstinence – the act or practice of restraining oneself from indulging in something.
- Depressant– a drug that reduces bodily functioning or instinct (ex. Tranquilizers, Klonopin, or Xanax.
- Hallucinations – perception like experiences that occur with an external stimulus; vivid/clear, involuntary, and can occur in all levels of sensation.
- Hallucinogen – a drug that causes hallucinations (ex. PCP, Ketamine and Peyote).Harm Reduction – a set of strategies aimed at reducing negative consequences from drug use. Also hold a belief in/respect for the rights of the people who use drugs.
- Inhalants – vapors introduced to the body by breathing it in (ex. Paint thinners and many household chemicals).
- Stimulant – a substance that increases attention, energy, heart rate, and respiration (ex. Cocaine and Ritalin).
- Opioids – a compound derived from the opium plant (ex. Morphine, methadone, and heroine).
Definitions retrieved via Dictionary.com (2017), unless otherwise noted
But, as you head into the social work profession you may find often times that the terms addiction, substance use, substance abuse, and dependency may be used interchangeably or be used to refer to the same thing. For example, the term “addiction” or “addict” can be seen on government websites whereas DSM-5 employs the term “substance use disorder”. These words are explaining the same events, symptoms, and treatments but from two different professional standpoints, the medical (government) person centered.
The goal of the DSM-5, as well as the social work profession, is to mitigate or prevent the self-imposed and social stigmas that can result from being labeled as “an addict.” By limiting harmful stereotypes and using person centered language (i.e. saying someone has a disorder rather than calling them an addict), the client may view the disorder as a manageable part of their life rather than being all of who they are. This is an important concept for social workers to be sensitive to and it is with that in mind that this chapter will use the term Substance Use/Substance Use Disorder.
Substance Use Disorder (SUD)
Substance use disorder (SUD) is a cluster of cognitive, behavioral, and physiological symptoms indicating that the individual continues using the substance despite significant substance related problems.
There are four key criteria that people must meet to be considered as having a Substance Use Disorder are impaired control, social impairment, risky use, and pharmacological criteria.
All information and statistics following are from the DSM-5 unless otherwise indicated.
SUDs include but are not limited to things such as:
● Alcohol Use Disorder is defined by a cluster of behavioral and physical symptoms, which can include withdrawal, tolerance, and craving. The prevalence of this disorder is very common in the United States with an 8.5% rate among those 18 years and older.
● Cannabis Use Disorder consist of behavioral and physiological symptoms that result from a long or heavy duration of cannabis use. This use disorder will often co-occur with other, more severe, substance use disorders like alcohol, stimulants or hallucinogens. While the full prevalence may be underreported, a study by Hasin et al. (2015) reveal that three out of ten (30%) marijuana users will qualify as having a use disorder.
● Hallucinogens are any drug that can produce alterations in perception and mood (See: Key Terms). Across a twelve-month span, it is estimated about 0.5% of the adult United States population will report symptoms of this disorder.
● Inhalants are classified as any substance that people only consume through inhaling. The result of this type of use is a mind-altering nature. Inhalants include things like gasoline, aerosol spray, or prescription medicines called nitrites (National Institute on Drug Abuse, 2017). This use disorder is most common in youth with about .4% of 12-17-year-olds reporting misuse although 10% of 13-year-olds do report using inhalants at least once.
● Opioids are a class of drugs that include the illegal drug heroin as well as legal drugs like morphine and codeine. These drugs deliver pain relief and euphoria when consumed. The consumption of prescribed opiates like morphine or OxyContin, becomes a substance use disorder when the opioids are consumed outside of a controlled environment or through self-administered dosages. In the United States, the prevalence of opioid use disorder is approximately 0.37% in adults.
● Stimulant use disorder is an abuse of substances like cocaine or methamphetamines. Symptoms of this disorder include cravings for stimulants, failure to control use when attempted, spending a great deal time obtaining and using stimulants, and withdrawal symptoms that occur after stopping or reducing use (SAMHSA, 2015)
● Tobacco use disorder occurs in people who use tobacco products in greater amounts or longer durations than originally intended. There is a strong desire to consume tobacco, increase intolerance to nicotine, and people may be unsuccessful at quitting tobacco products. The prevalence in the United States of tobacco use disorder is 13% (DSM-5, 2013) – a substantial number considering the estimated 66.9 million smokers of tobacco products (SAMHSA, 2015).
Substance Use Practice Settings
A social worker choosing the field of substance treatment will find themselves in two primary settings: inpatient and outpatient. Similar to the practice settings of mental disorders, substance use clinicians can work in inpatient clinics that house people trying to alleviate themselves of their substance use as well as enhance their health, an example of this can be seen in the film 28 Days starring Sandra Bullock. These types of facilities may have individual or group counseling sessions, provide drug screens, and provide time for the individual to reflect on their situation (Davis, 2013).
Outpatient clinics are another option for practice settings. These facilities offer potential clients scheduling flexibility and are not as intensive or hands on as inpatient facilities. These types of facilities allow clients to receive services like counseling, education, medication and support information at their own pace (AddictionCenter.com, 2017).
Current Issues
In 2017 there is a current drug use trend in the United States referred to as the Opioid epidemic. According to the Centers for Disease Control and Prevention (CDC) (2017), the majority of drug overdose deaths in the United States, six out of ten, in fact, involve some form of an opioid. This epidemic appears to be rooted in the use of prescription opiates. According to CDC statistics, nearly half of the opioid overdoses in the United States were linked to prescription pills like OxyContin, Methadone, and Vicodin (CDC, 2017).
But what happens when the person who has been using prescription opioids can no longer afford them? They turn to heroin. According to CNN reporter, Dr. Sanjay Gupta (2016), the price for heroin is almost one tenth the price per milligram than it is for a prescription. This may be one of the many reason we see such a rise in heroin use and, is often the case, death. They may also experiment with more dangerous drugs, such as fentanyl, as has been the case of the residents of Ohio (Opiate Action Team, 2017).
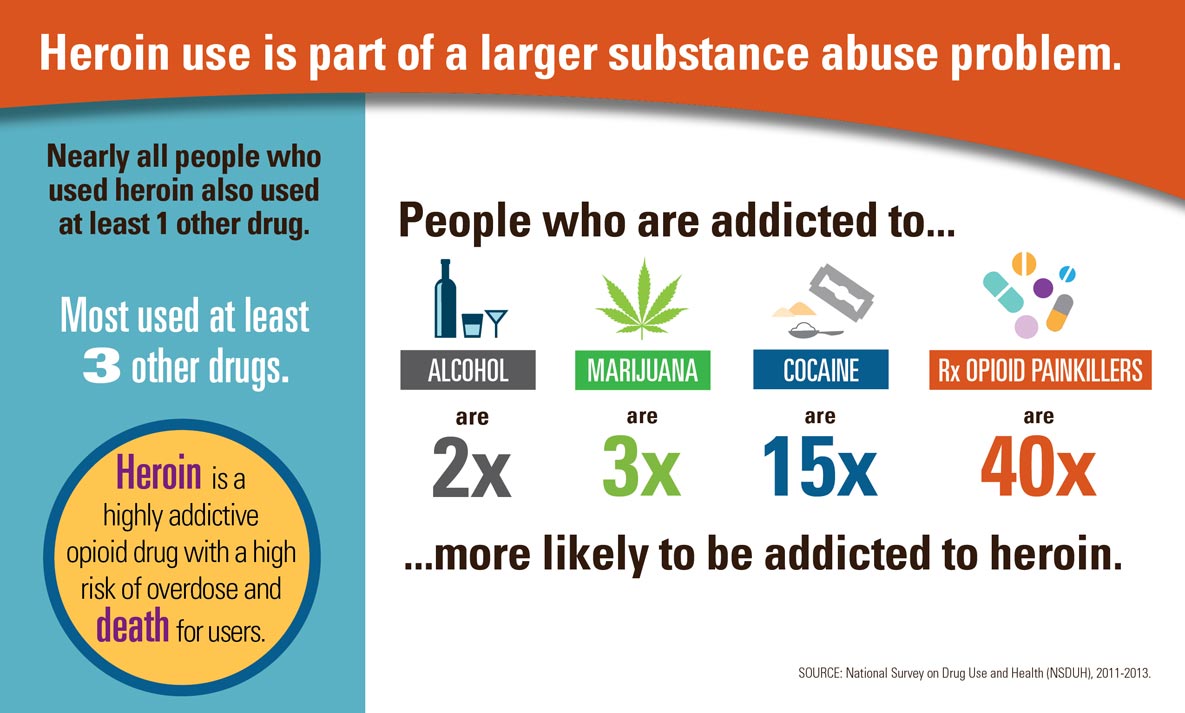
This increased trend in drug use has impacted a wide range of people and demographics, many of whom were never at “serious” risk for drug abuse before, like women, people with higher incomes, and the privately insured. Statistics show that 45% of people who used heroin were also addicted to some form of opiate painkiller (CDC, 2017).
Similar trends and concerns to that of Ohio can be seen across the United States.
https://www.hhs.gov/opioids/about-the-epidemic/index.html
The above links provide examples of the impacts and strategies that people and agencies dealing with the dramatic impact that opioids are currently having, not just on the country but all over the world. According to a White House press release titled President Trump’s First Budget Commits Significant Resources to Fight the Opioid Epidemic (2017), in the next year alone, the U.S. government will spend 12.1 billion dollars for treatment and prevention efforts. The U.S. will also provide 500 million dollars in grants so that states can work to reduce misuse, improve treatment, and increase access to treatment.
Social workers are at the forefront of combating this epidemic. Workers are meeting clients in hospitals as they recover from overdoses, counseling those seeking rehabilitation, work with insurance companies to distribute proper funds and ensure correct coverage, as well as educating youth on the dangers of opiates.
Philosophies of Treatment
As we can see, there is a large spectrum of substances that have different effects on the body and brain. If you choose to enter the field of substance treatment, you are bound to encounter different ways organizations or practitioners choose to treat their clients. Two main philosophies of substance treatment are Abstinence and Harm Reduction.
Some places may encourage the practice of abstinence. You may have heard this term regarding alcohol or sex because abstinence is defined as “the act or practice of restraining oneself from indulging in something” (Oxford Living Dictionaries, 2017). Some substance use treatment programs like Alcoholics Anonymous (AA) promote this type of behavior (DualDiagnosis.org, 2017).
According to Principles of Harm Reduction (2017), harm reduction, like many practices throughout social work, has the base philosophy of meeting people “where they are at” when it comes to their substance use. When working with a person who is suffering from a drug use problem (change the word problem) the social worker acknowledges that drugs are a part of part of this world, in both positive and negative terms (i.e. medications and illegal drugs). Rather than attacking or condemning the patient’s behavior, the clinician works with the person to minimize the use as well as the harmful effects of these substances thereby reducing the overall harm that is being done.
Both strategies have their limitations. For example, is it reasonable to ask someone to abstain without relapsing? How does a relapse impact the individual’s recovery? Will it be condemned or understood as part of healing? Can a person really get clean if they are still on a substance? Do we continually tolerate relapse or establish consequences for the undesired behavior? How much time is the counselor and client willing to take? Will the approach be safe for the client to participate in?
According to DualDiagnosis.org, 30% of people who participate in harm reduction or moderation type programs will end up in an abstinence-only program. However, according to a study conducted across a 33-month period, the success rate of abstinence only programs is very low – 5.9% for females and 9% for males (Recovery: Abstinence vs. Moderation, 2017). However, there is a current trend in this area of treatment moving more toward the use of interventions with evidence of effectiveness but information is currently limited.
Mental Disorder and Substance Abuse
Whether you are a social worker in mental health or substance treatment, inpatient or outpatient, there is an almost guarantee that you will encounter people who have both a mental disorder and substance use disorder in your career. This is referred to as a dual diagnosis where the presence of a mental disorder occurs along with the use of a substance.
According to the National Institute on Drug Abuse (2017), people who have a substance use disorder are nearly twice as likely to also be diagnosed with either a mood or anxiety disorder. However, a mental disorder can also lead to substance use in a sort of chicken vs. egg situation. For example, let’s say there is someone who has a diagnosis of depression who also uses a stimulant to try to alleviate it. Or perhaps someone has a diagnosis of alcohol use disorder and because of this use, they have developed depression. These are two potential examples of a dual diagnosis.
Case Study: Katie
Katie is a 26-year-old female. She has come into services due to a previous suicidal attempt. Her initial assessment gives her a diagnosis of Major Depressive Disorder and a secondary assessment of Alcohol Use Disorder. She remembers drinking since she was about 12 years old; she reports that she drinks to lessen the feelings of “sadness and feeling down.” She also reports that she feels “just as bad, if not worse” if she stops the drinking.Katie has attempted services in the past but discontinued them because she says, “I was fine after about 10 months of being with them so I stopped taking my medication and wanted to get on with my life.” Katie reports that she has a boyfriend who is very supportive and a mother in town. Her father is out of the picture but Katie reports he also had a history of substance use.
Consider how you would approach this case: What are some things you would want to know? What would you address first? Why? Feel free to discuss this in class.
As you can see, it takes a discerning professional to figure out the best path of treatment, plan for change with the individual, provide supports, assist in maintaining healthy coping, and a vast array of other tasks and responsibilities.
Things to Be Aware Of
Mental disorders and substance use are more common than people would like to admit. It adversely impacts many parts of people’s lives, whether directly or indirectly.
If you, or someone you know, is experiencing any signs or symptoms of a mental disorder or experiencing substance use please contact:
These websites are only an example of the many resources and supports available to people seeking help or assistance in navigating difficult life changes.
As a social worker in these fields, your role will be to help clients through these, potentially difficult, times. You will connect their clients to local resources, advocate for best practices to achieve client goals and outcomes, and offer non-judgmental supports to their clients. You yourself may even be that resource that people contact for individual therapy/counseling, or group therapy/counseling.
Techniques, Tools, and Strategies
Social workers can seek several avenues to assist their clients. As you may already be aware, social work strives to institute evidence based practice (EBP) when dealing directly with clients. These practices may include Cognitive Behavioral Therapy, Dialectical Behavioral Therapy, or Motivational Interviewing.
Social workers must also be familiar with medications that have been prescribed for treatment and their potential benefits, drawbacks, or chance for abuse (i.e. opiates).
Social workers working in inpatient settings may also help guide their clients through the process of detox. This process can be a long, painful, arduous process for many people and the support that a caring social worker can provide is an invaluable resource.
Social workers may lead support groups. These are organizations, generally outpatient, where clients gather to share their stories, successes, setbacks, hopes, and needs as they recover or maintain their mental or physical health regarding their disorder or substance use.
Finally, it behooves the social worker to know the person they are assisting. Establishing rapport, trust, and familiarity with the client’s personality, lifestyle, family structure, culture, and environment are invaluable pieces of information. The impact that a mental disorder or substance use disorder can have on these different systems are not isolated to one; rather these systems impact each other.
For example, someone experiencing a substance use disorder may withdraw from work or family functions seeking out isolation. They may make friends with similar substance use disorders, thereby creating a new environment that encourages the behavior. The person then may not have the support to seek positive change when they decide to finally pursue help.
Similarly, someone who is diagnosed as paranoid schizophrenic may not be able to function in their working environment. This lack of employment may impact their social circles and places of enjoyment, even where they now shop. This change in lifestyle may, in turn, impact family dynamics. The family, once a great support, may now be uninformed, resentful, or frightened of the sudden change in their loved one. The rejection of family may then have an impact on the belief in oneself to recover, cope and maintain their mental health.
Career Outlook
The area of social work that specifically deals with mental disorders and/or substance use has been around for decades and shows no signs of slowing down. In 2014 the number of social workers employed in the mental health and substance use fields was 117,800. The field is projected to add 22,300 jobs over the next 10 years, resulting in 19% job growth (U.S. Department of Labor, 2017).
Unfortunately, the Bureau of Labor Statistics (2017) also indicates that the social workers in the mental health and substance use fields tend to make less than their peers. Workers in mental health and substance use can expect to make an average of $42,700 compared to the top average pay of $60,230 from fields like private clinical or veterans administration workers. (NOTE: Payment tends to be degree dependent; those with BSW degrees tend to make less than those with MSWs.)
Summary
Social workers have, and will continue to, advocate for the understanding of and pursuit of social justice for some of the most misunderstood and vulnerable among us. These workers will encounter a variety of individual and co-occurring disorders in their profession.
Social workers in the mental health and substance use fields continue to improve treatment outcomes with a better understanding of the brain, trauma, and evidence based practice (EBP) models to provide treatment and care. These treatments can be in a variety of settings from community mental health (CMH) facilities, to hospitals, to private clinics.
There are many challenges in the country, as well as the world, and social workers are well equipped to combat many of these challenges going forward. This field will continue to grow over the next decade although the funding and pay scale for services is currently in question.
References
AddictionCenter.com. (2017). Outpatient drug rehab. Retrieved from https://www.addictioncenter.com/treatment/outpatient-rehab/>
American Psychiatric Association (APA). (2013). Diagnostic and statistical manual of mental disorders: DSM-5. Washington, DC: American Psychiatric Association.
American Psychiatric Association (APA). (2015, November). What is mental illness? Retrieved from https://www.psychiatry.org/patients-families/what-is-mental-illness
Anxiety and Depression Association of America (ADAA). (2016, August). Facts and statistics. (2016). Retrieved from https://adaa.org/about-adaa/press-room/facts-statistics
Bureau of Justice Statistics. (2017). Drugs and Crime Facts Retrieved from https://www.bjs.gov/content/dcf/enforce.cfm
Centers for Disease Control and Prevention (CDC). (2017, August 1). Prescription opioid overdose data. Retrieved from https://www.cdc.gov/drugoverdose/data/overdose.html
Davis, J. F. (2013, July 24). Day-to-day life during inpatient drug rehab. Addictionblog.org. Retrieved from http://drug.addictionblog.org/day-to-day-life-during-inpatient-drug-rehab/
DeepDiveAdmin. (2015, December 2). Case studies. PSYWeb.com. Retrieved from http://www.psyweb.com/casestudies/casestudies.jsp
Depression and Bipolar Support Alliance (DBSA). (2016). Dual diagnosis and recovery. Retrieved from http://www.dbsalliance.org/site/PageServer?pagename=education_brochures_dual_diagnosis
Dictionary.com. (2017). Retrieved from http://www.dictionary.com/
DualDiagnosis.org. (2017). Recovery: Abstinence vs. moderation. Retrieved from http://www.dualdiagnosis.org/drug-addiction/recovery-abstinence-vs-moderation/
Gupta, S. (2016, June 2). Unintended consequences: Why painkiller addicts turn to heroin. CNN. Retrieved from http://www.cnn.com/2014/08/29/health/gupta-unintended-consequences/index.html
Harm Reduction Coalition. (n.d.). Principles of harm reduction. Retrieved from http://harmreduction.org/about-us-principles-of-harm-reduction
Hasin, D. S., Saha, T. D., Kerridge, B. T., Goldstein, R. B., Chou, S. P., Zhang, H., …Grant, B. F. (2015, December). Prevalence of marijuana use disorders in the United States between 2001-2002 and 2012-2013. JAMA Psychiatry, 72(12), 1-19. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5037576/
Martin, M. E. (2018). Introduction to human services through the eyes of practice settings (4th ed.). New York: Pearson.
National Alliance on Mental Illness (NAMI). (n.d.). Schizoaffective disorder. Retrieved from https://www.nami.org/Learn-More/Mental-Health-Conditions/Schizoaffective-Disorder
National Alliance on Mental Illness (NAMI). (2017). Mental health by the numbers. Retrieved from https://www.nami.org/Learn-More/Mental-Health-By-the-Numbers
National Institute on Mental Health (NAMI). (2016, April). Bipolar disorder. Retrieved from https://www.nimh.nih.gov/health/topics/bipolar-disorder/index.shtml
National Institute on Drug Abuse. (2017, February). Inhalants. Retrieved from https://www.drugabuse.gov/publications/drugfacts/inhalants
Oxford University Press. (2017). Oxford living dictionaries. Retrieved from https://en.oxforddictionaries.com/
Opiate Action Team, Ohio Governor’s Cabinet. (2017). Data & statistics. Retrieved from http://fightingopiateabuse.ohio.gov/Data-Statistics
PBS.org. (2014). Thirty years of America’s drug war: A chronology. Frontline. Retrieved from http://www.pbs.org/wgbh/pages/frontline/shows/drugs/cron/
Substance Abuse and Mental Health Services Administration (SAMHSA). (2015, October 27). Mental and substance use disorders. Retrieved from https://www.samhsa.gov/disorders/substance-use
United States Department of Labor, Bureau of Labor Statistics. (2017). Social Workers. Occupational outlook handbook, 2016-17. Retrieved from https://www.bls.gov/ooh/community-and-social-service/social-workers.htm
The White House, Press Office. (2017, May 23). President Trump’s first budget commits significant resources to fight the opioid epidemic [Press release]. Retrieved from https://www.whitehouse.gov/the-press-office/2017/05/23/president-trumps-first-budget-commits-significant-resources-fight-opioid
Wisner, B. & Adams, J. (Eds.). Environmental health in emergencies and disasters: A practical guide. Geneva, Switzerland: World Health Organization (WHO), 2002. Retrieved from http://www.who.int/water_sanitation_health/hygiene/emergencies/em2002intro.pdf
Wolf, P. (2001). Creativity and chronic disease Vincent Van Gogh (1853 – 1890). Western Journal of Medicine, 175(5), 347-348. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1071623/pdf/wjm17500348.pdf
World Health Organization (WHO). (2017). Substance abuse. Retrieved from http://www.who.int/topics/substance_abuse/en/

