4.4 Objective Assessment
Objective assessment involves the collection of data that you can observe and measure about the client’s state of health. Examples of objective assessment include observing a client’s gait, physically feeling a lump on client’s leg, listening to a client’s heart, tapping on the body to elicit sounds, as well as collecting or reviewing laboratory and diagnostic tests such as blood tests, urine tests, X-ray, etc. Typically, an objective assessment is conducted following the collection of subjective data.
The purpose of the objective assessment is to identify normal and abnormal findings. The abnormal findings are cues that signal a potential concern. An important part of the nursing process to ensure client safety and effective care is:
- Recognizing abnormal cues.
- Acting on abnormal cues.
Failing to recognize or act upon abnormal cues can lead to significant negative consequences for the client.
Objective data are analyzed in combination with your subjective assessment to make a clinical judgment. A clinical judgment is the outcome of thinking critically about the data, analyzing the cues as a whole, making decisions about the most significant concerns to address, and identifying how to best address these concerns based on the existing evidence (National Council of State Boards of Nursing, 2018). As a health care professional, developing strong clinical judgment is essential to ensuring client safety and maintaining your competency. Your clinical judgment will guide the prioritization and sequencing of assessment techniques. Your assessment of cues (both subjective and objective) will help you determine what data warrant further investigation and assessment. Therefore, it is important to think critically about the findings you collect during an assessment: Are they normal or abnormal for this specific client? Do they require you to act and/or seek further assistance?
Clinical Tip
Recognizing and acting on assessment findings
As a nursing student, you must have timely discussions with your clinical instructor or preceptor to assess the significance of abnormal findings. You will need to take initiative, develop confidence in seeking assistance, and never ignore an abnormal finding.
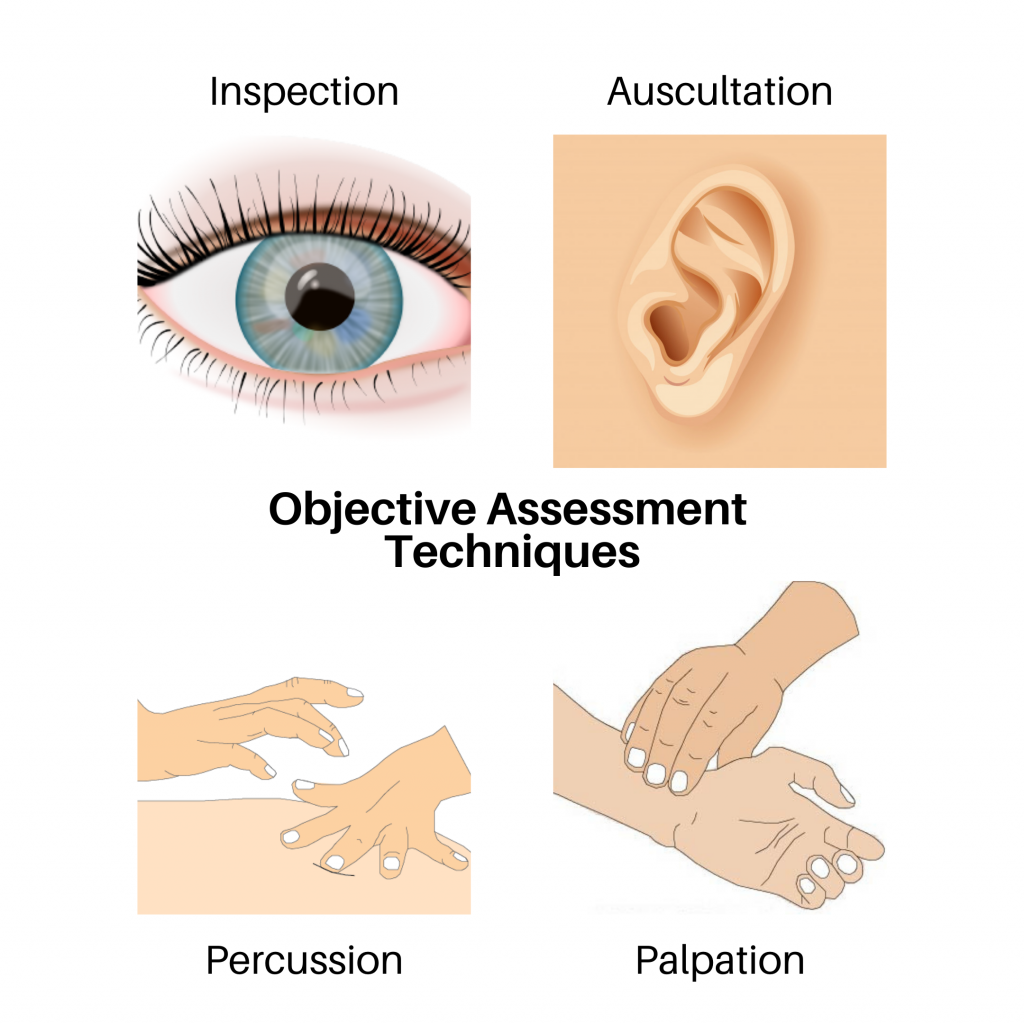
In this chapter, you will focus on four objective assessment techniques: inspection, palpation, percussion, and auscultation. These involve your senses of sight, hearing, and touch (see Figure 4.1). You should also be aware of your sense of smell when conducting any physical assessment, as certain odors can act as a cue; for example, a foul odor may indicate an infection.
- Inspection involves your visual sense to observe the client.
- Palpation involves your sense of touch to physically feel areas of the body.
- Percussion involves a combination of touch and hearing, but your focus is on hearing sounds when tapping the areas of the body.
- Auscultation involves your sense of hearing while listening to areas of the body with a stethoscope.
These techniques should be performed with methodical and deliberate action. Always perform inspection first because it is the least invasive and does not involve physical touch. Inspection also allows you to establish a baseline for your assessment. For example, if you observe someone crouched over in pain, this will inform the sequence of your subsequent assessment techniques. Typically, palpation, percussion, and then auscultation follow inspection. The sequencing of techniques may be rearranged for several reasons, including which system is being assessed and for safety reasons. For example, when assessing the abdomen, auscultation is generally performed before percussion and palpation. Client safety and comfort also influence the sequence of objective techniques. For example, with a sleeping infant, you should perform inspection and auscultation while the child is calm and avoid awakening the client. You will learn more about modifications to the sequencing of techniques as you learn about specific body systems. Determining technique sequence also comes with experience.
When applicable, these IPPA techniques are used to assess body systems (e.g., eyes, ears, heart and neck vessels, lungs and thorax, abdomen, musculoskeletal). However, not all techniques are applicable to all systems. For example, you would not auscultate an eye because it does not emit a sound that would give you relevant data. Additionally, developmental stage and age can influence how some IPPA techniques are performed and also the determination of normal and abnormal findings. For example, normal heart rates vary significantly between a newborn and an adult.
Before you explore each technique, let’s discuss what you need to do before you begin the objective assessment!
Voices of Experience
Your foundational IPPA assessment techniques and the resultant findings will give you a baseline understanding of the client’s health status. These physical assessment skills, combined with subjective health assessment, are important parts of clinical judgment and can act as a prompt for urgent action, transfer to a higher level of care, and further diagnostic technologies. Your IPPA assessment skills will be even more important in areas with less access to resources and diagnostics (e.g., rural and remote areas and underdeveloped regions).
Attribution
This section contains material taken from The Complete Subjective Health Assessment by Jennifer Lapum, Oona St-Amant, Michelle Hughes, Paul Petrie, Sherry Morrell, and Sita Mistry and is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.

