15.9 Breasts: Inspection and Palpation
Examination is usually completed in a seated position facing the examiner. The client is instructed to place hands on hips and also instructed to raise hands above head, allowing inspection from different positioning of the breasts.
Inspection of Breasts
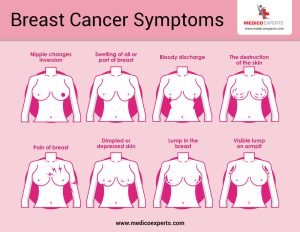
Inspect the breasts for symmetry, shape, size, and color. Inspect the nipple size, shape, direction, texture, and color.
Visually inspect the breasts while the patient is sitting and lying down. Ask the patient to raise their arms above their head, let them hang by their sides, or press their hands against their hips.
-
- Look for differences in breast size, shape, symmetry; and nipple size, shape, texture, and color.
- Check for areas of skin thickening, dimpling, or fixation relative to the underlying breast tissue.
- Look for rashes, fluid, or discharge leaking from the nipple, or nipple changes such as inversion or scaling.[1]
The steps for this are as follows:
1. Identify any presence and location of skin thickening, dimpling, fixation, visible mass, or unilateral nipple inversion or discharge.
- These findings are often associated with breast cancer and require precise documentation using the clock method. The clock method is a systematic way to document the location of a breast lump. This method uses the analogy of a clock face to describe where a lump is located within the breast. It helps health care providers communicate clearly about the lump’s position.
2. Note the color.
- Areas of thickening or orange-peel appearance can appear darker than surrounding skin. Recent unilateral nipple or areola color changes noted as darker or lighter from surrounding area. Presence of vasculature often described as bluish.
Palpation of Breasts
Patient Positioning:
-
- The patient should lie down on the examination table with one arm raised behind the head on the side being examined.
- A small pillow or folded towel can be placed under the shoulder to flatten the breast tissue.
Palpation Technique
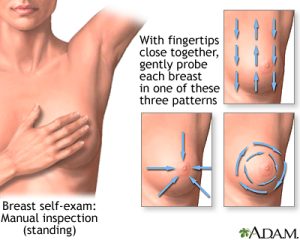
- Use of Pads of Fingers:
- Use the pads of the middle three fingers to palpate the breast.
- Apply different levels of pressure (light, medium, and deep) to feel all layers of breast tissue.
- Systematic Pattern:
- Use a systematic pattern to ensure the entire breast is examined. Common patterns include the vertical strip, concentric circles, and radial spoke methods.
Palpation Patterns
- Vertical Strip Pattern:
- Start at the outer edge of the breast and move in a vertical line up and down.
- Move from the collarbone to the bra line and from the sternum to the armpit.
- Cover the entire breast in small, overlapping vertical strips.
- Concentric Circles Pattern:
- Begin at the outermost edge of the breast and move in small, circular motions.
- Gradually move inward in concentric circles towards the nipple.
- Ensure each circle overlaps with the previous one.
- Radial Spoke Pattern:
- Start at the outer edge of the breast and move inwards towards the nipple in a straight line.
- Return to the outer edge and move inwards again, covering the breast like the spokes of a wheel.
- Ensure all areas are palpated, including the upper outer quadrant, which is where most breast cancers are found.
Specific Areas to Palpate
- Upper Outer Quadrant:
- Pay special attention to the upper outer quadrant, which extends into the armpit area (the tail of Spence), as it is a common site for breast cancer. Check the entire breast, underarm, and collarbone area for any changes or abnormalities, such as lumps. Palpate to three levels of depth: superficial, medium, and deep/to the level of the chest wall**
- Nipple and Areola:
- Palpate the tissue beneath the nipple and areola.
- Gently compress the nipple to check for discharge.
- Axillary Region (Underarm):
- Palpate the axillary lymph nodes by pressing gently into the armpit.
- Check for any enlarged or tender lymph nodes.
- Supraclavicular and Infraclavicular Areas:
- Palpate above and below the clavicle to check for any swollen lymph nodes.
Identify the presence, location, size, shape, texture and description of any masses, lesions, and lymph nodes.
- If you identify any mass, lesion, or lymph node, ask the client whether they have noticed it, how long they have had it, whether they know the cause, and if they have treated it with anything.
- These findings are often associated with breast cancer and require precise documentation using the clock method. The clock method is a systematic way to document the location of a breast lump. This method uses the analogy of a clock face to describe where a lump is located within the breast. It helps health care providers communicate clearly about the lump’s position.
5. Note the findings.
-
- Normal findings might be documented as: “Breasts symmetrical in size and shape, skin smooth and even in color, firm, uniform consistency, no lumps or masses palpated, no tenderness noted. Nipples everted, no discharge, areolae evenly pigmented, no lesions.”
- Abnormal findings might be documented as: “Left breast larger than right, redness noted on the upper outer quadrant of the right breast. Firm mass palpated in the upper outer quadrant of the left breast, approximately 2 cm in diameter, tender to touch. Dimpling observed on the lower inner quadrant of the left breast, peau d’orange appearance noted. Right nipple retracted, crusting present around the left nipple, slight bloody discharge from the right nipple.”
Priorities of Care
When a patient presents with a new breast lump, it is important to address both the physical and psychological aspects of care. Here are the priorities of care for managing a new breast lump:
- Take a detailed medical history, including personal and family history of breast cancer or other cancers.
- Conduct a clinical breast exam to assess the lump’s size, shape, texture, location, and mobility.
- Check for other symptoms such as nipple discharge, skin changes, or lymph node enlargement.
- Encourage questions and provide detailed answers to alleviate anxiety.
- Emotional Support:
- Acknowledge the patient’s feelings and concerns.
- Provide reassurance and support throughout the diagnostic process.
- Offer counseling or referral to a mental health professional if needed.
Support Systems:
- Encourage the involvement of family or friends for emotional support.
- Provide information about support groups for individuals dealing with breast lumps or breast cancer.
Knowledge Bites
While breast cancer is more common in women, men can also develop it. Early detection and awareness are crucial for both. Gynecomastia is a condition characterized by the enlargement of breast tissue in men; it is often caused by hormonal imbalances and can occur at various life stages. Regular self-examinations help individuals detect any unusual changes, such as lumps or discharge, early on. This practice is essential for both men and women. Routine check-ups and mammograms (for women over 40 or with a family history of breast cancer) are important preventive measures.
Breasts often carry cultural and personal significance related to femininity, masculinity, and body image. Acknowledge and respect diverse perspectives and experiences. For transgender men, women, and non-binary people, breasts may have different roles and significance. Understanding and respecting these experiences is vital for supportive health care and social interactions.
- OpenAI. (2024). ChatGPT. [Large language model]. https://chat.openai.com/chat. Content was reviewed by the authors for accuracy. ↵

