11.13 Auscultation of the Apical Pulse
Auscultation of the heart involves auscultating the apical pulse followed by auscultating the valves of the heart. You must always cleanse the stethoscope prior to auscultating. After you have cleansed it, do not set it down on the table or wrap it around your neck because this will contaminate it.
Extraneous noises can be heard when in a noisy environment or with a client who has a hairy chest. Thus, it is important to reduce environmental noise if possible and keep your stethoscope still when you press it against the chest.
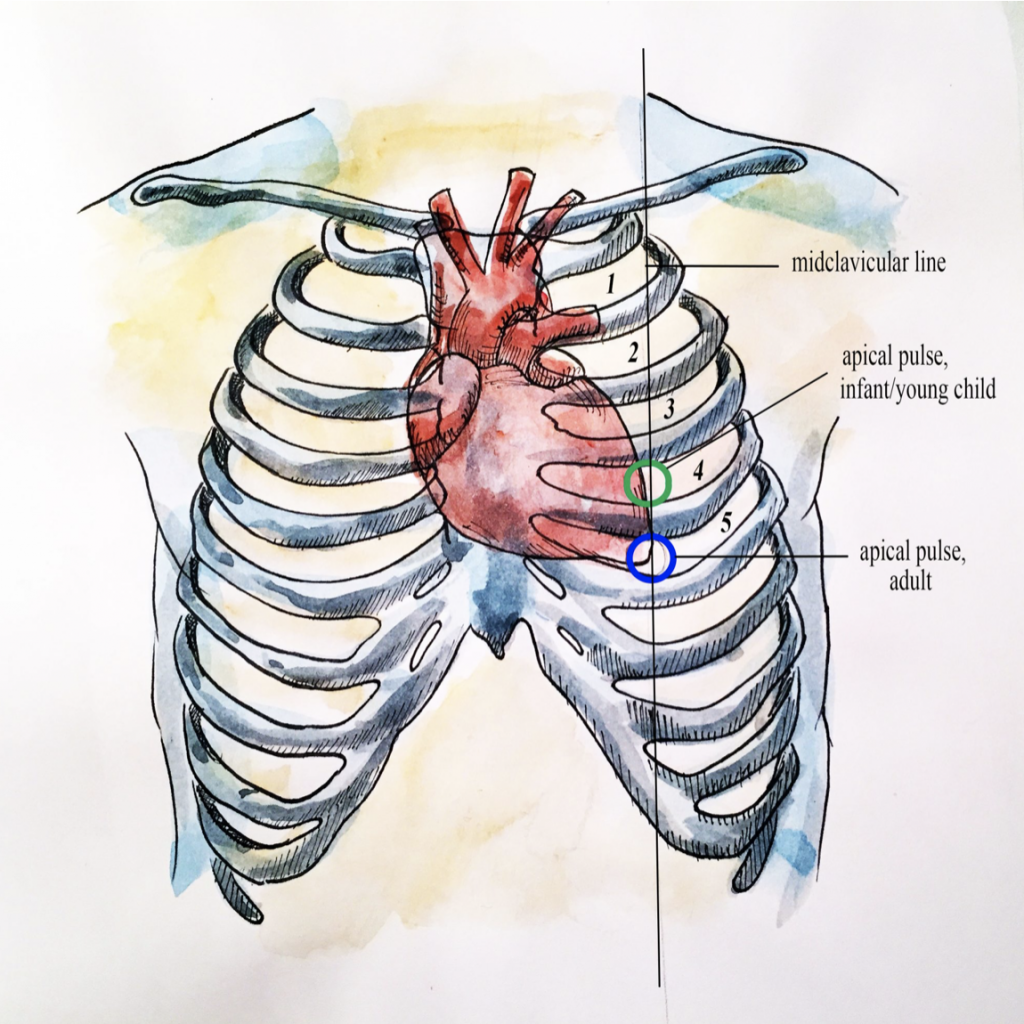
Auscultation of the apical pulse involves assessing the rate and the rhythm. This is best done at the apex, which is landmarked at the 5th intercostal space (for adults) and the 4th intercostal space (for children) at the left midclavicular line. See Figure 11.7.
Auscultation of the apical pulse involves the following steps (see Video 11):
Step 1: Keep the client in a supine position and continue to drape.
- This procedure can also be completed in a sitting position.
Step 2: Cleanse the stethoscope.
Step 3: Physically landmark the location of the apical pulse.
Step 4: Place the diaphragm of the stethoscope at the correct location with a complete seal.
Step 5: Count the rate for one minute and report beats per minute.
- One beat is considered one cardiac cycle (systole and diastole) and it sounds like “lub dub.” Lub correlates with the closure of the AV valves and is referred to as S1; it signals the beginning of ventricular contraction (systole). Dub correlates with the closure of the SL valves and is referred to as S2; it signals the beginning of ventricular relaxation (diastole).
- Apical pulses are typically counted for a full minute to assess for any irregularities.
Step 6: Note the rhythm (e.g., regular or irregular rhythm).
- Normally, the rhythm is regular which means there is an even tempo with equal intervals between beats.
- If the rhythm is irregular, note whether it is a regularly irregular rhythm or an irregularly irregular rhythm.
- Regularly irregular rhythm: a regularity to the irregular rhythm, for example three regular beats and one missed beat and then this pattern is continually repeated.
OR
-
- Irregularly irregular rhythm: an irregularity to the irregular rhythm, for example there is no pattern to the irregular rhythm. For example, you might hear two beats in a row, 1 missed beat, three beats in a row, 1 missed beat, 1 beat etc… This irregular rhythm is more concerning. When it is irregularly irregular, it is an erratic rhythm in which the heart is not always fully contracting at systole and filling with blood at diastole. This type of rhythm is highly specific to atrial fibrillation, in which the atria quiver. This can result in blood clots and decreased stroke volume and cardiac output. As a result, it can also lead to the heart not optimally perfusing blood to the periphery.
- If the rhythm is irregular, check for a pulse deficit. A pulse deficit is when the radial pulse is less than the apical pulse, meaning that you will feel fewer palpable pulses at the radial site compared to the number of beats heard when auscultating the apical pulse. Normally there is no pulse deficit when a heart is perfusing the periphery. Experts suggest that a pulse deficit of more than 10 should be investigated further, particularly when associated with other symptoms. To assess for a pulse deficit, use the following steps:
- While auscultating the apical pulse, also palpate the radial pulse. You can usually do this at the same time and note whether they are equal.
- If they are unequal, count the apical pulse for one minute, and then count the radial pulse for one minute. Next, subtract the radial pulse from the apical pulse to obtain the client’s pulse deficit. For example, if the apical pulse is 90 beats per minute and the radial pulse is 72 beats per minute, you would calculate the pulse deficit as 18 beats per minute (90 – 72 = 18), meaning that those 18 times that the heart contracts, the blood is not being perfused to the periphery.
Step 7: Note the findings.
- Normal findings might be documented as (example): “Apical pulse 82 beats per minute with a regular rhythm.”
- Abnormal findings may be documented as (example): “Apical pulse 134 beats per minute with an irregularly irregular rhythm.”[1]
Video 11: Auscultation of apical pulse.
Priorities of Care
Notify the physician/nurse practitioner if a client has an irregularly irregular rhythm and is showing signs of bradycardia or tachycardia. Additionally, a pulse deficit is of concern because it is suggesting that the heart is not perfusing the periphery. Thus, you should perform a full cardiac assessment. Unless the client is showing signs of clinical deterioration and requires prompt intervention, you should first complete a full cardiac assessment so that you can provide a full report of the relevant cues and share recommendations for actions.
ANSWER: The apical pulse rate in Video 11 is 82 beats per minute.
- Content adapted from https://wtcs.pressbooks.pub/nursingskills/chapter/9-3-cardiovascular-assessment/) ↵

