6.2 Introduction to the Integumentary System
The integumentary system includes the skin, hair, nails, and sebaceous and sweat glands. It has important functions including thermoregulation, sensory functioning, ensuring fluid balance, serving as a protective barrier to external substances, and providing immune defense against foreign bodies.
The integument can be an indicator of the client’s general health status. For example, the integumentary system can signal other systemic functions of the body, like diaphoresis during cardiac events, cyanosis related to respiratory insufficiency and other conditions, and pallor during times of stress and other conditions. As a nurse, it is important to hone your assessment skills and pay close attention to potential cues that may signal underlying concerns that require your intervention. See Figure 6.1 for an anatomical overview of the integumentary system.
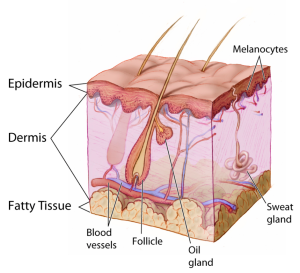
You have already learned about the anatomy and physiology of the integumentary system. View The Science of Skin for for a quick overview.
You need a basic understanding of disease-specific presentations to effectively interpret findings from your assessment. Be alert to signs and symptoms of greater systemic issues that may require further assessment and possibly immediate intervention. For example, Cullen’s sign (Figure 6.2) is a serious concern: it appears as bruising and edema of the subcutaneous fatty tissue around the navel and can be an indication of acute pancreatic trauma and/or internal bleeding. Certain skin symptoms can also prompt the use of personal protective equipment (PPE); for example, small flat red spots that appear on the face and spread down the body may be an indication of measles (Figure 6.3), necessitating airborne precautions.


Contextualization of integumentary issues in relation to other symptomatology like fever, cough, and inflammation can provide insight into underlying conditions. Table 6.1 provides some general descriptions related to the integument and underlying pathophysiology. With experience, you will learn to identify patterns, recognize cues, and begin to discriminate between benign skin conditions and skin conditions that require further investigation.
| Integumentary grouping | Examples | Common presentation |
| Skin trauma
Trauma can affect a single or multiple layers of the skin as a result of injury or illness. |
Burns, scars, cuts, tears of the skin, keloids (thick, raised scars).
Keloid. Photo by Htirgan – Own work, CC BY-SA 3.0. |
Swelling, erythema, inflammation, bleeding, pain, blisters, peeling of skin, and sometimes darkened or lightened areas of skin with scars. |
| Infections
Bacterial, viral, fungal, and parasitic skin infections are caused by various pathogens and can range from mild to severe. Many skin infections require treatment.
Shingles. Photo by James Heilman, MD – Own work, CC BY-SA 3.0. |
Viral: Human papillomavirus (HPV), herpes zoster virus, warts, COVID-19, shingles.
Bacterial: Staphylococcus aureus, Methicillin-resistant Staphylococcus aureus (MRSA), impetigo, cellulitis, boils, and abscesses. Fungal (typically skin and mucosal surfaces): Tinea corporis (ringworm), tinea pedis (athlete’s foot), candidosis (yeast infection), nail fungus. Parasitic: Lice, bedbugs. Other stings and bites that can cause infection: Spider bites, ticks, animal bites.
Tick bite with bull’s-eye rash (an early sign of Lyme disease). CDC / James Gathany, Public Domain. |
Viral: Some rashes can follow a dermatome (e.g., shingles, varicella, herpes simplex) with lesions, papules, or pain. They can appear in cluster/closely grouped or as a single lesion, and can be generalized, regional, or asymmetrical presentation (i.e., rash on one side of the body).
Bacterial: Odor, exudate, small red bumps increasing in size, fever, yellowish-brown crusts, redness, heat, swelling, tenderness, pain. Fungal: Deep erythema, swelling, itchiness, scaly, flaky patches, or loss of normal pigmentation of the skin causing discoloration. Parasitic: Itchiness, rash, regional lymphadenopathy (diseases of the lymph nodes resulting in enlarged lymph nodes). |
| Auto-immune and/or inflammatory disorders causing lesions/eruptions (acute and chronic)
Regional or generalized; may involve inflammation of the skin. |
Psoriasis, eczema, seborrheic dermatitis, vitiligo, lupus, alopecia.
Alopecia. Photo by Abbassyma at English Wikipedia – Transferred from en.wikipedia to Commons, Public Domain. |
Eczema (scaling, itching, ill-defined), psoriasis (well-demarcated, scaly plaques), vitiligo (depigmentation, patchy loss of skin color, premature whitening of hair), alopecia (hair loss). |
| Metabolic and nutritional disorders
Poor nutrition or absorption issues can lead to vitamin deficiencies. Excess vitamins can also lead to cutaneous abnormalities. |
Vitamin A, C, D, E, K, B1, B2, B3, B6, B9, B12, iron, zinc, and selenium deficiencies.
Vitamin A, E, and selenium excess. |
Varies depending on metabolic/nutritional disorders, e.g., dermatitis, flushing, hyperpigmentation, white spots. |
| Vascular disorders
Cutaneous vascular disorders commonly involve arteries, veins, and/or lymphatic vessels. |
Ulcers, cherry angiomas, venous insufficiency.
Venous insufficiency. Photo by Ashashyou – Own work, CC BY-SA 4.0.
Cherry angioma. |
Varies depending on venous insufficiency (flooding of fluid to the skin due to inadequate venous return) or arterial deprivation (deprivation of nutrients to the skin due to poor arterial perfusion).
Variations such as cherry angiomas are not harmful. They can begin small and then grow in size, become slightly raised, and multiply over time. |
| Psychological and neurological disorders
Involve interactions between the mind and skin. |
Persistent pruritus and prurigo, neuropathic pain (often related to shingles), trichotillomania (a psychiatric condition resulting in compulsive hair pulling). | Irresistible itching and scratching, urge to scratch exacerbated by anxiety, skin picking, recurrent pulling out of hair. |
| Systemic disorders
The integumentary system can be involved in clinical manifestation of some systemic disorders. |
Gout, arthritis, Addison disease, Cushing syndrome, thyroid disease, chronic liver disease, hepatitis, diabetic ulcers. | Varies depending on the underlying systemic disorder.
Gout. Photo by Gonzos ft – Own work, CC BY 3.0. |
| Neoplastics (abnormal growths) and cancer
Benign cutaneous neoplasms are very common. Some abnormal growths are benign (non-cancerous). However, some neoplasms become malignant and require intervention. |
Benign: Freckles, lentigo, café-au-lait spots, nevi, seborrheic keratosis, wart, cutaneous cysts.
Malignant: Atypical nevi, basal cell carcinoma, squamous cell carcinoma, melanoma.
Seborrheic keratosis (the large brown raised lesion). |
Varies depending on the underlying cause, e.g., spots on the skin, palpable mass, depression of the skin.
Basal cell carcinoma.
Photo by James Heilman, MD – Own work, CC BY 3.0. |
| Skin disorders caused by external agents
Cutaneous adverse reactions can occur because of reactions to drugs or other external agents. Adverse reactions can also occur from heat and cold exposures. |
Steven-Johnson syndrome and toxic epidermal necrolysis are rare life-threatening skin disorders where the skin peels and blisters, often caused by medications and infections. Toxic erythema from chemotherapy is a skin reaction including eruptions of red/purple rash and plaques. Photosensitivity is a skin sensitivity when exposed to the sun caused by medications like chemotherapy drugs, HIV medications and antibiotics, frostbite. |
Skin reactions, like rashes, that start after exposure to external agents, like medications. |
*genetic disorders not listed
Clinical Tip
Did you know that some dermatological conditions are emergencies? For example, necrotizing fasciitis (a rare bacterial infection also known as flesh-eating disease) can spread very quickly throughout the body, at a rate of 1 inch per hour. Symptoms include erythema, warmth to the touch, swelling, severe pain, and fever. If not treated immediately, it can lead to sepsis, shock, organ failure, and even death. As a nurse, you must report these findings to the physician or nurse practitioner so immediate treatment can be started.
Knowledge Bites: Pathophysiology
How do you distinguish between common viral and bacterial infections? Common characteristics of a bacterial infection are inflammation, exudate (such as pus), erythema, swelling, pain, and odor. Common characteristics of a viral infection are a grouping/cluster of lesions, generally asymmetrical (one side of body), and on specific regions of the body (e.g., mouth, nose, feet, hands).
Activity: Check Your Understanding
Name the integument pathophysiology images:
Use the checklist below to review the steps for completing an “Eye and Ear Assessment.”
Steps
Disclaimer: Always review and follow agency policy regarding this specific skill.
- Gather supplies: penlight, Ishihara plates, Snellen chart, Rosenbaum card, or a newspaper to read.
- Perform safety steps:
- Perform hand hygiene.
- Check the room for transmission-based precautions.
- Introduce yourself, your role, the purpose of your visit, and an estimate of the time it will take.
- Confirm patient ID using two patient identifiers (e.g., name and date of birth).
- Explain the process to the patient and ask if they have any questions.
- Be organized and systematic.
- Use appropriate listening and questioning skills.
- Listen and attend to patient cues.
- Ensure the patient’s privacy and dignity.
- Assess ABCs.
- Use effective interview questions to collect subjective data about eye or ear problems.
- Inspect the external eye. Note any unexpected findings.
- Assess that pupils are equally round and reactive to light and accommodation (PERRLA).
- Assess extraocular movement.
- Inspect the external ear. Note any unexpected findings.
- Assess distance vision acuity using the Snellen eye chart and proper technique.
- Assess near vision acuity using a prepared card or newspaper.
- Asses for color blindness using the Ishihara plates.
- Assess hearing by accurately performing the whisper test.
- Assist the patient to a comfortable position, ask if they have any questions, and thank them for their time.
- Ensure safety measures when leaving the room:
- CALL LIGHT: Within reach
- BED: Low and locked (in lowest position and brakes on)
- SIDE RAILS: Secured
- TABLE: Within reach
- ROOM: Risk-free for falls (scan room and clear any obstacles)
- Perform hand hygiene.
- Document the assessment findings. Report any concerns according to agency policy.










