14.6 Oral Cavity: Inspection and Palpation
Usually the client is positioned sitting upright; newborns or young children can be held by their parent/caregiver. Wear gloves because this assessment involves contact with body fluids from the mucus membranes. You will also need a tongue depressor and a penlight.
Inspection of Lips
Inspect the lips for swelling, color, lesions, or malformations. Also inspect the lips for moisture and texture, which are interrelated.
The steps for this are as follows:
1. Identify any presence and location of swelling and redness.
- These two findings are often associated. You must respond immediately if you suspect the swelling is associated with anaphylaxis. For example, do they have allergies, such as food or bees, or have they recently had a vaccine? Do they have other signs of anaphylaxis (e.g., hives, pruritus, dyspnea, dysphagia, tachycardia, hypotension)?
2. Note the color.
- Lip color varies based on the client’s skin color. It can range from pink to brown tones. Note any lip discoloration (e.g., redness, cyanosis, pallor). Cyanosis can appear as a gray/white shade in people with darker skin (Lewis, 2020; Sommers, 2011) or as a dusky bluish/purple shade in people with lighter skin (Lewis, 2020). Pallor can appear as a gray shade in people with darker skin (Lewis, 2020) or as a generalized pale discoloration in people with lighter skin.
3. Identify the presence, location, size, and description of any lesions and malformations, including the color and presence of any discharge.
- If you identify a lesion, ask the client whether they have noticed it, how long they have had it, whether they know the cause, and if they have treated it with anything.
- A common lesion on the lips is herpes simplex virus (cold sore), which appears as small, fluid-filled blisters; see Figure 14.2. Another common malformation of the lip is a cleft lip (which is sometimes associated with a cleft palate). These are important to assess and act upon because they can affect a client’s breathing, speaking, and sucking and swallowing associated with eating. They are often surgically repaired at a young age. Further information and images for cleft lip and palate can be found at the CDC website.
- Are the lips moist or dry? Moist lips are smooth with no cracking. Dry lips are chapped and/or may have fissures. Chapped lips are flaky and sometimes red, with “flakes” or “scales” of skin peeling away from the lips. Fissures are usually called “cracked lips.”
- Normal findings: “Lips are moist with no cracking, lesions, or swelling, pink in color with generalized brown tones, no discoloration.”
- Abnormal findings: “Lips are dry with cracking, a red lesion on upper lip left of midline 3mm x 3 mm with a slight serous discharge.”

Inspection of Oral Mucosa
Systematically inspect all parts of the mucosa. Shine a penlight in the mouth to illuminate the area. You can ask the client to pull their top lip up and then their bottom lip down, or use a gloved hand or tongue depressor to perform this action so you can inspect the mucosa on the inside of the lips.
Most clients can open their mouth wide and tip their head back so that you can observe the palate and also put the tip of their tongue behind their front teeth so that you can observe the floor of the mouth and under the tongue. You can use a tongue depressor to expose the buccal mucosa. To expose the pharynx, ask the client to stick their tongue out and say “ahhh” or pretend to yawn. You may need to use the tongue depressor to press the tongue down. If so, avoid using it in the middle of the tongue as this may elicit a gag reflex.
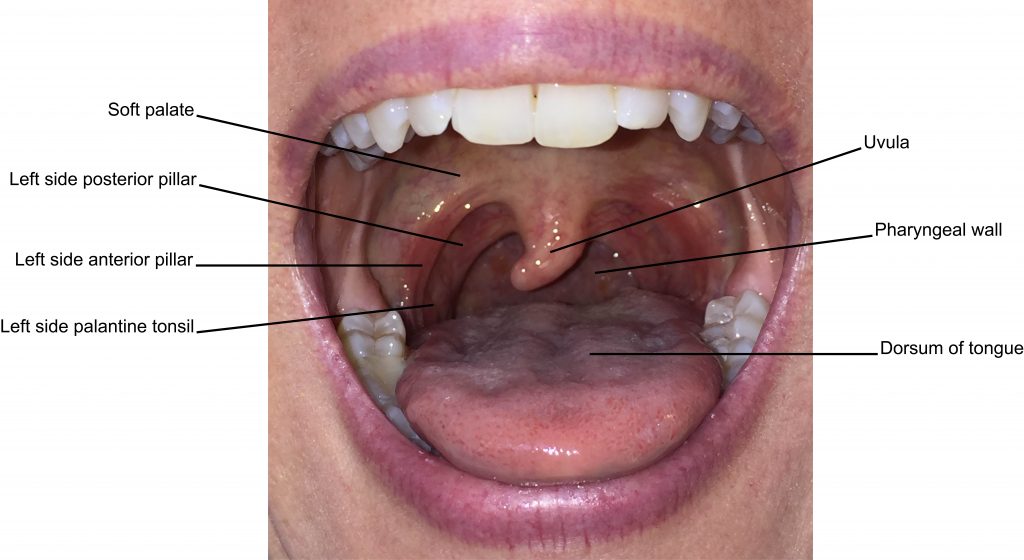
Inspection of the mucosa of the oral cavity includes observing the insides of the lips and the buccal mucosa (inside of checks), the tongue, the floor of mouth (under the tongue) and the hard and soft palate, the pharynx, and salivary glands. See Figure 14.3 for anatomical locations of the oral cavity.
Use the following steps:
1. Note moisture or dryness.
- The whole oral cavity should be moist. Dry mucous membranes are often a sign of dehydration. However, you should also assess if the client may be a person who breathes through their mouth and not their nose. You will notice tiny ductal openings (about 1 mm in size) of the salivary glands. These glands produce saliva for the mouth and include the parotid (ductal opening on the buccal mucosa near the upper second molar), the submandibular (ductal opening at the base of the ventral surface of the tongue on both sides of the frenulum), and the sublingual (several ductal openings on both side of the floor of the mouth).
2. Inspect the mucosa of the lips and buccal mucosa for color, lesions, swelling, and nodules.
- The mucous membranes, including the mucosa of the lips and buccal mucosa, are pink in color. Any discolorations (e.g., cyanosis or pallor) should be described and the location noted. Cyanosis can appear as a gray/white shade in people with darker skin (Lewis, 2020; Sommers, 2011) or as a dusky bluish/purple shade in people with lighter skin (Lewis, 2020). Pallor appears as a gray shade in people with darker skin or as a generalized pale discoloration in people with lighter skin.
- The mucosa of the lips and buccal mucosa are intact with a smooth surface. Note the description and location of any lesions, swelling, or nodules. Palpate any lesions, swelling, or nodules and identify the consistency (e.g., soft or hard).
3. Inspect the tongue, floor of the mouth, and hard and soft palate for color, lesions, swelling, nodules, and malformations.
- Note the color and any discolorations along with the location. The tongue is normally pink with a dotted surface that is most readily seen on the dorsal and posterior side. The small and hard palate are a lighter pink in which the hard palate (directly behind the upper front teeth) has a slight white shading. The ventral surface of the tongue is highly vascular, and you will observe veins under the tongue.
- The mucosa is normally intact with a smooth texture except the hard palate, which has a ridged surface. Note the description and location of any lesions, swelling, nodules, or malformations. Palpate any lesions, swelling, or nodules and identify the consistency (e.g., soft or hard). One of the most common malformations at birth is a cleft palate.
- While doing so, observe for halitosis, which refers to a bad odor. It is important to recognize that “stale” smelling breath is not necessarily a concern and also to understand that this can be embarrassing for clients. Therefore, it is important to approach the situation in a sensitive manner. There are many causes of halitosis that should be assessed. For example, common causes are dehydration, bacteria associated with poor oral care, diabetes, tobacco, and recent ingestion of foods such as garlic, onion, and coffee.
4. Inspect the pharynx for color, swelling, lesions, and nodules, and describe the tonsils.
- Note the color and any discolorations (such as redness or white patches) along with the location.
- Identify the presence, location, and description of any swelling, lesions, or nodules.
- Note the size of both the left and the right tonsil. Sometimes tonsils have been surgically removed so they may not be present, but usually tonsils are just visible to view. Many “scales” are used to grade tonsil size, but there is no one standardized scale. Therefore, it is better to describe the size as in the following examples:
- Tonsils are not present.
- Tonsil(s) is visible between the anterior and posterior pillar, but not enlarged.
- Tonsil(s) is enlarged at halfway between the anterior pillar and the uvula.
- Tonsil(s) is enlarged and touching the midline of the mouth or the uvula. (If both tonsils are enlarged, you may describe them as touching each other.)
5. Note the findings.
- Normal findings might be documented as: “Moist oral cavity. Pink mucosa with no discoloration, lesions, nodules, or swelling. Tonsils are visible but not enlarged.”
- Abnormal findings might be documented as: “Dry mucous membranes of oral cavity. White, raised patches on the tongue, buccal mucosa, soft palate, and pharynx.”
Teeth and Gums
Assessment of the teeth and gums includes inspection and palpation. Use a penlight to illuminate the back of the mouth. Begin by asking the client to smile to expose the teeth, and use a tongue depressor or your gloved finger to expose the gums and the back teeth. Remember: your assessment of the teeth and gums does not replace a routine dental assessment.
Assessment of the teeth and gums involves the following steps:
1. Inspect the color of the teeth.
- Tooth enamel is white, so you should note any discoloration. When enamel begins to erode, teeth may have a yellowish color, which reflects the underlying layer, and even a brown color. Enamel erosion and tooth discoloration can be caused by many things including smoking, diet (e.g., red wine, coffee/tea), bruxism, decay, and acids introduced into the mouth as a result of bulimia. Some mild erosion is associated with aging due to exposure to cultural factors such as diet.
2. Inspect for missing, chipped, or broken teeth.
- Note the presence and location.
3. Inspect for missing or loose fillings.
- Note the presence and location.
4. Inspect the gums for color, swelling, and bleeding.
- Identify the presence and location of any discoloration such as redness, swelling, or bleeding. Healthy gums have a pink color similar to the buccal mucosa, with no swelling or bleeding.
5. Palpate for loose teeth and palpate the gums for pain.
- Use your gloved finger to palpate for the presence of any loose teeth, and note the location.
- Next, use your gloved finger to palpate the gums for pain while using the tongue depressor to pull the buccal mucosa out. Ask the client if they feel any pain or tenderness and note the location.
6. Note the findings.
-
Normal findings might be documented as: “White teeth with no loose, missing, chipped, or broken teeth. Gums are pink in color with no swelling, bleeding, or pain.”
- Abnormal findings might be documented as: “Slight yellow discoloration of the teeth. Second molar on upper right side loose with swelling of the gum and mild bleeding.”
Priorities of Care
Respond immediately if a client has swollen lips consistent with other signs of anaphylaxis (e.g., hives, pruritus, dyspnea, dysphagia, tachycardia, hypotension). If so, did they just receive a vaccine or were they exposed to an allergen (e.g., a food or bee sting) that they are allergic to? If so, call for help and notify the physician/nurse practitioner immediately. If you are permitted to do so, administer epinephrine. Continue to monitor the client because anaphylaxis is life-threatening.
If the client shows signs of cyanosis or pallor, perform a primary survey (ABCCS) to assess for clinical deterioration. Usually a client with discolorations in lips or mucous membranes will have other respiratory- or cardiovascular-related cues such as dyspnea, low oxygen saturation, tachypnea, and/or angina.
If the client has dry and cracked lips and dry mucous membranes with no other signs of dehydration, increasing fluid intake will usually resolve the issue. This could involve administering a rehydration solution that contains electrolytes; other forms of fluid intake can include ice chips (or popsicles for children), especially if the client is nauseated.
Further assessment and intervention may be needed if signs of more advanced dehydration are observed: poor skin turgor, oliguria, dark urine, altered level of consciousness, tachycardia, and hypotension. With newborns and infants, you should assess for sunken fontanelles, decreased wet diapers, and drowsiness. An infant may also show reduced or absent tears when crying. For a hospitalized client with signs of advanced dehydration, perform a primary survey to assess for signs of clinical deterioration, increase intravenous fluids to rehydrate, and treat any other related symptoms such as diarrhea, vomiting, and fever. Report any cues that suggest clinical deterioration to the physician/nurse practitioner.
Lesions, nodules, discolorations, and enlarged tonsils are not usually urgent priorities for treatment, but you should complete a focused assessment (subjective and objective) to document them and report your findings to the physician/nurse practitioner. If tonsils are enlarged, you should assess the color and the presence of exudate. If tonsils are touching the uvula or each other, you should assess for any breathing or swallowing issues. These associated symptoms require prompt intervention. Any issues associated with teeth (particularly loose, broken, or chipped teeth or missing or loose fillings) and gums usually require referral to a dentist. You should be concerned when the client indicates they have a lesion in their mouth that will not heal or a lump. These can sometimes be associated with oral cancers, which are commonly found on the floor of the mouth, inferior side of tongue, the buccal mucosa or the soft palate. A common cause of oral cancers is tobacco use.
Knowledge Bites
This image shows a throat infection called tonsillitis. Evidence of the infection is shown through swelling, redness and white patches (pus) on the tonsils. This pus consists of dead bacteria, white blood cells, and cellular debris.


