Interpersonal Violence: Global Impact and Paths to Prevention
Attention to interpersonal violence as a global issue has expanded dramatically since the World Health Assembly identified violence as a public health priority in 1996. Reports by the United Nations (UN) have contributed greatly to increased awareness (Krug and others 2002; Pinheiro 2006; UN 2006). These and other efforts culminated in specific targets for eliminating interpersonal violence in the UN’s post-2015 Action Agenda for Sustainable Development (UN 2015).
Nature and Burden of Interpersonal Violence
Globally, the three primary forms of violence are interpersonal violence; self-directed violence, including suicide; and collective violence, including war, terrorism, and state-perpetrated violence in the form of genocide or torture (Dahlberg and Krug 2002). This chapter focuses on interpersonal violence.
Definitions of Interpersonal Violence
The World Health Organization (WHO) defines violence as follows: “The intentional use of physical force or power, threatened or actual, against oneself, another person, or against a group or community that either results in or has a high likelihood of resulting in injury, death, psychological harm, mal-development, or deprivation” (Dahlberg and Krug 2002, 5). This definition encompasses interpersonal, self-directed, and collective violence.
Interpersonal violence involves the intentional use of physical force or power against other persons by an individual or small group of individuals. Interpersonal violence may be physical, sexual, or psychological (also called emotional violence), and it may involve deprivation and neglect. Acts of interpersonal violence can be further divided into family or partner violence and community violence.
-
Family or partner violence refers to violence within the family or between intimate partners. It includes child maltreatment, dating and intimate partner violence (IPV), and elder maltreatment.
-
Community violence occurs among individuals who are not related by family ties but who may know each other. It includes youth violence, bullying, assault, rape or sexual assault by acquaintances or strangers, and violence that occurs in institutional settings such as schools, workplaces, and prisons.
The Burden of Interpersonal Violence
Information on the magnitude, nature, and consequences of interpersonal violence is critical for program and policy development.
Deaths Resulting from Interpersonal Violence
WHO’s Global Health Estimates (GHE) indicate that approximately 1.4 million people died in 2011 as a result of all three major forms of violence (table 5.1). Of those deaths, 35.3 percent, or 504,587, were due to interpersonal violence. GBD estimates find that 83 percent of all violence-related deaths occur in low- and middle-income countries (LMICs), and 91.4 percent of deaths due to interpersonal violence occur in LMICs. In 2011, the estimated rate of deaths due to interpersonal violence or homicide in LMICs was 8.0 per 100,000 people, compared with 3.3 per 100,000 in high-income countries (HICs).
Rates and patterns of violent death varied by region (figure 5.1). Homicide rates were highest in LMICs in Latin America and the Caribbean and in Sub-Saharan Africa, and lowest in East Asia and the Pacific and in some countries in northern Africa. In 2010, homicide was the leading cause of years of life lost in tropical and central Latin America, the fourth leading cause in southern Sub-Saharan Africa, and the eighth leading cause in the Caribbean and Eastern Europe (Lozano and others 2012). Poorer countries, especially those with large gaps between the rich and the poor, tend to have higher rates of homicide than wealthier countries (Butchart and Engstrom 2002).
Homicide rates differed markedly by age and gender (table 5.2). For infants and young children ages 0–4 years, the rates for male and female homicide victims are 2.9 and 3.2 per 100,000, respectively; this is the only age range in which the female rate exceeds the male rate. For the 15- to 29-year-old age group, rates for males were nearly five times those for females; for the remaining older age groups, rates for males were around two to four times those for females. Homicide rates for females doubled between the ages of 5–14 and 15–29 years and then decreased; however, the rates increased again in women ages 70 years and above. Rates for males increased almost tenfold for males 15 to 29, declined slightly for those 30 to 49, and then decreased with age. Overall, homicides resulted in the deaths of slightly more than 4 males for every 1 female. Recent estimates indicate that, globally, about one in seven homicides, and more than one in three homicides of females, are perpetrated by an intimate partner (Stöckl and others 2013).
Firearms are associated with a substantial number of homicides around the world. In 2010, an estimated 196,200 firearm homicides were committed in nonconflict situations (Lozano and others 2012). Firearm suicides are also an important problem in many countries, such as in the United States, where more than 60 percent of all firearm deaths are suicides. The number of suicides committed with firearms globally is unknown.
Nonfatal Interpersonal Violence
In recent years, multiple reports using household survey data have characterized the prevalence of interpersonal violence.
Violence against Children and Youth
Results from the United Nations Children’s Fund (UNICEF) Multiple Indicator Cluster Surveys and Demographic and Health Surveys (DHS) in 33 countries found that an average of 76 percent of children ages 2 to 14 years had experienced some form of violent physical or psychological discipline during the previous month (UNICEF 2010). Surveys of violence against children in five countries (Haiti, Kenya, Swaziland, Tanzania, and Zimbabwe) found that the prevalence of sexual violence against girls was 26 percent to 38 percent, and against boys it was 9 percent to 21 percent (CDC, INURED, and the Comité de Coordination, 2014; Reza and others 2009; UNICEF, CDC, and KNBS 2012; UNICEF, CDC, and Muhimbili University 2012; ZIMSTAT, UNICEF, and CCORE 2012). The prevalence of physical violence against girls was 61 percent to 74 percent, and against boys it was 57 percent to 76 percent. The prevalence of emotional violence against girls was 24 percent to 35 percent, and against boys it was 27 percent to 39 percent. Regardless of the type of violence, perpetrators are largely known to the victim, and violence tends to occur in homes.
In meta-analyses of studies worldwide, 11 percent to 22 percent of girls and 4 percent to 19 percent of boys have experienced child sexual abuse, 14 percent to 55 percent have experienced child physical abuse, 12 percent to 22 percent have experienced physical neglect, and 13 percent to 25 percent have experienced emotional neglect (Stoltenborgh and others 2011; Stoltenborgh and others 2013a; Stoltenborgh, Bakermans-Kranenburg, and van Ijzendoorn 2013b). The hidden nature of child sexual and physical abuse is poignant. When compared with official reports, self-reported prevalence of child sexual abuse was more than 30 times the official rate (Stoltenborgh and others 2011); self-reported prevalence of physical abuse was more than 75 times the official rate (Stoltenborgh and others 2013a).
In youth ages 10 to 24 years, interpersonal violence was the fifth leading cause of disability-adjusted life years (DALYs) in 2004, accounting for 3.5 percent of all DALYs in this age group (Gore and others 2011). Unfortunately, few studies in LMICs examine the nonfatal consequences of youth violence. This research gap urgently requires filling.
Violence against Women
The prevalence of violence against women has been documented by Demographic and Health Surveys conducted in Sub-Saharan African countries (Cameroon, Kenya, Malawi, Rwanda, Uganda, Zambia, and Zimbabwe) and by Reproductive Health Surveys (RHS) conducted in Central and South American countries (Ecuador, El Salvador, Guatemala, Jamaica, Nicaragua, and Paraguay). In Sub-Saharan Africa, the DHS findings show that the prevalence of physical violence against women ranged from 30 percent in Malawi to 60 percent in Uganda, with most perpetrators being intimate partners; the prevalence of sexual and emotional violence by intimate partners was also high (Borwankar, Diallo, and Sommerfelt 2008). For Central and South America, RHS findings show prevalence of physical violence against women ranging from 17 percent in Jamaica to 31 percent in Ecuador (Bott and others 2012). Global and regional estimates of violence against women demonstrate that 35 percent of women worldwide have experienced physical or sexual violence (or both), and most of that violence was perpetrated by intimate partners (WHO 2013).
Violence against Elderly People
Elder maltreatment has been examined using population-based surveys and records from adult protective services. In surveys, 6.0 percent of older people reported significant abuse in the past month, and 5.6 percent of couples reported physical violence in their relationship in the past year (Cooper, Selwood, and Livingston 2008). In studies involving vulnerable elders in nursing or care homes, nearly 25 percent reported significant levels of psychological abuse. Rates of abuse reported to adult protective services are generally very low (1 percent to 2 percent).
Consequences of Interpersonal Violence
The consequences of experiencing interpersonal violence are pervasive and enduring. Evidence confirms that exposure to violence increases the risks of injuries, infectious diseases, mental health problems, reproductive health problems, and noncommunicable diseases (NCDs).
Cause of Physical or Psychological Injury
Although injury historically has been defined as an individual’s experience of physical damage, the definition has been expanded to include damage that is psychological, with the potential to lead to maldevelopment or deprivation (Norton and Kobusingye 2013). Whether they are physical or psychological, violence-associated injuries commonly go unrecognized and range from self-limiting to severe. Physical injuries include lacerations, bruises, wounds, fractures, broken teeth, ocular damage, burns, internal injuries, and head injuries. Such injuries, especially those associated with highly lethal means such as firearms, may lead to disability, including brain damage, amputations, or paralysis (Buchanan 2013).
Link to Infectious Diseases
The association between sexual and physical violence and infectious diseases, particularly sexually transmitted infections (STIs) and human immunodeficiency virus/acquired immune deficiency syndrome (HIV/AIDS) is well supported. Evidence across multiple studies demonstrates that these associations are strong, largely consistent, graded, and biologically plausible (Andersson, Cockcroft, and Shea 2008; Machtinger, Wilson, and others 2012). Emerging evidence suggests that violence may be associated with the transmission and progression of infections, increases in antiretroviral failure, high-risk behaviors, and an independently elevated risk of HIV/AIDS-associated death (Machtinger, Haberer, and others 2012). The importance of gender-based violence as a driver of HIV/AIDS in women is so prominent that multilateral donors such as UN Women view elimination of violence against women and children as a key strategy for advancing prevention (IOM 2013).
Increased Risk of Reproductive Problems
Multiple studies document the reproductive consequences of exposure to child maltreatment and IPV. These forms of violence are associated with unintended pregnancy and teen pregnancy, and they influence victims’ associated risk behaviors, such as multiple partners and early initiation of sexual activity (Hillis and others 2004). The intergenerational effects of exposure to childhood violence may be extreme. For example, violence against girls increases the future risk of adverse pregnancy outcomes, such as fetal death (Hillis and others 2004). In addition, mortality for young children is significantly higher when their mothers are victims of IPV (Silverman and others 2011). A review of studies from 17 LMICs shows that IPV leads to an increased prevalence of pregnancy-associated mental health disorders, such as postpartum depression, which impair a mother’s ability to provide a safe, stable, and nurturing environment for her children (Fisher and others 2012).
Increased Risk of Mental Health Problems
Globally, studies from high-, middle-, and low-income countries document that violent experiences lead to various mental health consequences. The WHO World Mental Health Survey findings from 21 countries demonstrate that violence during childhood is associated with mood, anxiety, behavior, and substance disorders, as well as suicidal behavior, during adulthood (Kessler and others 2010). Furthermore, studies involving 21,000 women from Asia, Sub-Saharan Africa, and Latin America and the Caribbean confirm strong associations between various forms of violence—including experiencing and witnessing IPV, nonpartner physical violence, and childhood sexual abuse—and suicides (Devries and others 2011).
Increased Risk of Future Violence
Exposure to violence during childhood increases the risk of experiencing or perpetrating violence later in life. Experiencing child maltreatment and witnessing partner abuse have consistently been shown to increase the risk of becoming either a perpetrator or a victim of sexual violence and IPV as an adult (Capaldi and others 2012; Tharp and others 2012). This intergenerational effect of childhood violence increases the risk that men will become perpetrators and that women will become victims. An assessment of Reproductive Health Surveys in six countries in the Americas found that the proportion of women reporting IPV was more than twice as high for those who experienced sexual or physical abuse in childhood as for those who did not (Bott and others 2012).
Increased Risk to Special Populations
Although most reports addressing interpersonal violence focus on the general population, some recent studies have addressed infectious, reproductive, and mental health consequences of violence for children outside of family care, including street children, trafficked children, those affected by crises and armed conflict, and those living in institutions such as orphanages. For street children, studies from LMICs report HIV/AIDS seroprevalences of 40 percent and higher among those who experienced childhood violence, in contrast to general population prevalences of 1 percent (Kissin and others 2007; Robbins and others 2010). Associations between violence and elevated risks of HIV/AIDS and STIs, pregnancy, psychiatric pathology, depression, anxiety, posttraumatic stress disorder, and suicide have been reported among victims of sex trafficking and armed conflict, as well as among those in orphanages (Reed and others 2012; Silverman and others 2009; Zapata and others 2011, 2013).
Increased Risk of NCDs
Violence during childhood is also associated with noncommunicable diseases (NCDs) that often only become evident decades later. Exposure to childhood violence leads to consistent and graded increases in the four NCDs that accounted for nearly 60 percent of the 53 million deaths globally in 2010—cardiovascular disease, cancer, chronic lung disease, and diabetes (Lozano and others 2012; Norman and others 2012). In both HICs and LMICs, childhood violence has been associated with major risk factors for these diseases, including alcohol abuse, tobacco use, physical inactivity, and obesity (Anda and others 2010). Beyond health effects, serious psychosocial effects of childhood violence that are observed decades later include severe problems with finances, family, jobs, anger, and stress (Hillis and others 2004).
Basic Science Evidence
The biological underpinnings of the empirical associations between exposure to violence and subsequent major causes of mortality in adulthood have been established through basic science. Recent evidence demonstrates that traumatic stress, such as that associated with violence in childhood, impairs brain architecture (both structure and function), immune status, metabolic systems, and cellular inflammatory responses (Anda and others 2010). It is clear that early exposure to toxic stress in childhood confers lasting damage at the most basic levels of the nervous, endocrine, and immune systems, and that such exposures can alter the physical structure of DNA (epigenetic effects) (Danese and McEwen 2012). Important research summarizing the effects of early childhood experiences suggests that those multifaceted gene-environment interactions that cause negative health consequences after exposure to chronic stress also appear to confer positive health consequences after exposure to early environments that are engaging and nurturing (Heim and Binder 2012). Epidemiologic research complements these findings, demonstrating that early nurturing in the home leads to sustained positive economic and psychosocial consequences up to five decades later (Hillis and others 2010).
Economic Burden of Interpersonal Violence
Given the high prevalence of interpersonal violence and its extensive consequences, the associated economic impact is substantial. However, no comprehensive framework for estimating the total economic burden of violence exists.
Framework for Estimating the Costs of Violence
Challenges in creating such a framework include “weaknesses in the knowledge base both in economic costing and in violence prevention, difficulty in creating a universal algorithm for diverse settings, and disagreements in types of costs to include” (IOM and NRC 2012, 7). Although no methodology exists to enumerate the full impact of violence, costs that are commonly considered include direct costs, which arise proximal to the violent event, and indirect costs, which result from consequences, externalities, or lost opportunities (IOM and NRC 2012). In general, direct costs typically include those associated with medical care, psychological care, property damage, policing, incarceration, and residential treatment; indirect costs are those commonly associated with lost wages and decreased productivity. Current approaches that largely confine estimates of health-related costs to proximal consequences lead to marked underestimates because they fail to incorporate costs of HIV/AIDS, chronic diseases, and other conditions attributable to violence.
A comprehensive approach to estimating costs will strengthen global efforts to elevate the urgency of violence prevention (WHO 2004). Comparisons across countries of the costs of interpersonal violence are complicated by variations in definitions, types of costs, discount rates, comparable data, and methodology. Reports vary greatly in the types of costs they include, whether such costs are disaggregated, and whether they include costs associated with both victimization and perpetration. Although the absolute costs appear to be higher in HICs than LMICs, the relative costs of violence as a proportion of government spending are often high in both types of economies (table 5.3).
Reports of direct and indirect societal costs of interpersonal violence in general vary widely, ranging from US$75.2 million (2013 dollars) for homicide in New Zealand in 1992 to US$579.4 billion (2013 dollars) for homicide, child abuse, sexual and other assault, and robbery in the United States in 1993 (Fanslow and others 1997; Miller, Cohen, and Wiersema 1996). Estimates of the costs of both interpersonal and collective violence in the Americas show that direct and indirect economic costs ranged from 5.1 percent of 1997 gross domestic product (GDP) in Peru to 24.9 percent of 1997 GDP in El Salvador (Buvinic, Morrison, and Shifter 1999). Other estimates found that interpersonal violence accounted for 4.0 percent of GDP in Jamaica in 2006, 1.2 percent in Brazil in 2004, and 0.4 percent in Thailand in 2005 (Butchart and others 2008; Ward and others 2009).
Reports that estimate the national costs of child maltreatment are largely from HICs, whereas those that address IPV also include LMICs. In HICs, for example, Fang and others (2012) estimated the U.S. total lifetime economic burden resulting from new cases of child maltreatment in 2008 to be US$135 billion (2013 dollars); an analysis using similar methods showed total costs of US$19.0 billion (2013 dollars) in Germany (Habetha and others 2012). HIC estimates of the annual direct and indirect costs of IPV against women exceeded US$8.9 billion in the United States and US$1.7 billion (all 2013 dollars) in Canada (CDC 2003; Day 1995). For LMICs, costs of the lost productive capacity of abused women as a percentage of GDP were equivalent to 2.0 percent in Chile, 1.6 percent in Nicaragua, and 22.0 percent in Morocco (table 5.3) (ICRW 2009; Morrison and Orlando 1999). Although adolescents and young adults commit a disproportionate share of all violence and, therefore, account for a high proportion of its cost, youth violence has been the subject of few economic cost studies (WHO 2004).
Risk and Protective Factors for Violence
Violence results from the interplay of risk factors and protective factors. In table 5.4 these risk factors are organized by levels of the ecological model, which examines the relationship between individual and contextual factors and considers violence as the product of these multiple levels of influence on behavior (Dahlberg and Krug 2001). Identifying these factors is important, because increasing protection and decreasing risk underlie effective prevention. Several cross-cutting risk factors for perpetrating violence are described in table 5.4. Many of these factors also increase an individual’s likelihood of being a victim; for example, young men ages 15 to 44 are most likely to be both victims and perpetrators in any country. Additional factors, such as having a disability (Hughes and others 2012), increase the risk of becoming a victim but not a perpetrator.
The recognition that different types of interpersonal violence share common risk factors, often occur in combination, and may be causal factors for one other is important (Reza, Mercy, and Krug 2001). For example, child maltreatment is a risk factor for youth violence and IPV. Three cross-cutting risk factors bear particular mention because they represent factors that, if successfully addressed by prevention initiatives, could have substantial impact: parenting, substance abuse (particularly alcohol), and the availability of lethal means.
Harsh, cold, and inconsistent parenting has been linked to youth violence (van der Merwe, Dawes, and Ward 2012), IPV (Ireland and Smith 2009), and the increased risk of abusing one’s own children (Thornberry, Knight, and Lovegrove 2012). In contrast, children who receive warm, consistent parenting tend to have better outcomes (Eisenberg and others 2005; Smith, Landry, and Swank 2010).
Substance abuse, and particularly alcohol abuse, is implicated in a number of ways in both victimization and perpetration of violence (Monteiro 2007; WHO 2006). Maternal use of alcohol during pregnancy can result in fetal alcohol spectrum disorders, with their attendant executive functioning disorders (Mattson and others 2013), which increase the risk of aggression in affected children. Alcohol use also reduces self-control and the ability to process information (Giancola 2000), making it more likely both that drinkers will use violence in response to perceived threats and that they will be vulnerable to victimization (Klosterman and Fals-Stewart 2006). Alcohol misuse has been implicated across all forms of violence, including perpetration of child maltreatment (Gilbert and others 2009) and elder abuse (Lachs and Pillemer 2004), and in both victimization and perpetration of youth violence (van der Merwe, Dawes, and Ward 2012) and IPV (Jewkes 2002).
Access to lethal means of perpetrating interpersonal violence, such as firearms and sharp objects, contributes substantially to the likelihood that such violence will result in death or serious injury (Beaman and others 2000). In the United States, the presence of a firearm in the home is associated with an increased risk of homicides, especially among women (Miller, Azrael, and Hemenway 2013). The same authors report that in cross-national comparisons of HICs, higher homicide rates have been associated with greater access to firearms.
Interventions and their Applicability to low- and Middle-Income Countries
Public health interventions aim to prevent violence from occurring. Prevention efforts addressing common underlying risk factors have the potential to decrease several different forms of violence simultaneously. Such efforts include two broad groups of interventions:
-
The first group targets documented risk and protective factors (for example, enhancing support for parents, reducing the availability and abuse of alcohol, and reducing access to lethal means) in well-defined target groups, such as adolescents. This group includes specific violence prevention programs implemented at the community, state and provincial, and national levels.
-
The second group consists of policies and programs that address the social determinants of violence, including efforts to improve the conditions of daily life and to promote more equitable distribution of power, money, and resources.
Policy makers understand that a single intervention or policy will not solve the whole problem, nor will one sector solve it alone; as with automobile safety, the solutions will be incremental and will require multisectoral collaboration among policy makers in criminal justice, public health, education, and other areas.
The design, targeting, monitoring, and evaluation of both groups of interventions are enabled by the availability of timely and reliable surveillance information about outcomes of interest, including homicides, nonfatal injuries treated in emergency departments, and self-reported violence recorded through surveys. Indeed, one program that has significantly reduced violence-related injuries in Cardiff, Wales, is based on the systematic sharing of anonymous data from hospital emergency rooms and the police to better identify high-risk locations for violence (Florence and others 2013). Such locations become the focus of situation-specific interventions to reduce risks, for example, by increasing the presence of police patrols at high-risk times where alcohol is served, altering practices around the serving of alcohol (such as the mandatory use of plastic barware), and instituting crowd control at public transportation stops.
Specific Violence Prevention Programs
Most of the scientific evidence for specific prevention programs to date is from HICs. Although conditions differ in LMICs, table 5.5 shows seven categories of violence prevention programs in HICs that are scientifically credible, along with the types of violence they prevent and considerations for their applicability in LMICs.
Developing Safe, Stable, and Nurturing Relationships between Parents or Caregivers and Children
Interventions that support the development of safe, stable, and nurturing relationships between parents or caregivers and children in their early years can prevent child maltreatment and reduce childhood aggression (Bilukha and others 2005; Kaminski and others 2008). Emerging evidence suggests that such relationships can also reduce violence in adolescence and early adulthood; theoretical grounds exist for assuming they decrease IPV and self-directed violence in later life (Caldera and others 2007; Olds and others 1998; Walker and others 2011). In addition, these relationships offer the potential to prevent problem behaviors, such as substance misuse, eating disorders, and unsafe sex, which are important risk factors for NCDs; STIs, including HIV/AIDS; and unintentional injuries.
Although most evidence for the effectiveness of parenting programs comes from HICs (Knerr, Gardner, and Cluver 2013; Mikton and Butchart 2009), several initiatives to evaluate such programs in LMICs have recently been established, for example, the Children and Violence Evaluation Challenge Fund. In addition, parenting programs are quite widely implemented in LMICs to support early child development, raising the possibility that violence prevention components could be integrated into those programs.
Developing Life Skills in Children and Adolescents
Social development programs to build social, emotional, and behavioral competencies can prevent violence (Hahn and others 2007; Hawkins and others 1999; Klevens and others 2009). Preschool enrichment programs that provide children with academic and social skills at an early age appear promising (Baker-Henningham and others 2012; Nelson, Westhues, and MacLeod 2003). However, outcomes vary greatly across programs, and relatively few programs have been evaluated for their effects on violence (Durlak, Weissberg, and Pachan 2010).
School-based programs can address gender norms and attitudes with the aim of preventing dating violence. The Safe Dates program in the United States (Foshee and others 2005) and the Youth Relationship Project in Canada (Wolfe and others 2009) are evidence-based approaches that could be adapted to LMICs. Life skills and social development training programs are popular in LMICs. Some include evaluations of effectiveness (for example, PREPARE in South Africa). However, because programs are typically delivered in schools, they depend on the readiness of the educational system to implement the program and reinforce its effects. Oversight and management structures must be in place before such programs are implemented.
Reducing the Availability and Harmful Use of Alcohol
Alcohol availability can be regulated by restricting the hours of sale and reducing the number of alcohol retail outlets (Cohen 2007; Duailibi and others 2007; Nemtsov 1998). Reduced hours of sales have been associated with reduced violence, and higher outlet densities have been associated with higher levels of violence. Empirical evidence has shown that higher prices for alcohol can decrease consumption and reduce mortality attributed to alcohol (Zhao and others 2013). Moreover, economic modeling suggests that price increases can reduce violence (Markowitz and Grossman 1998, 2000). Brief interventions and longer-term treatment for problem drinkers have been shown to reduce child maltreatment and IPV (Dinh-Zarr and others 2004). Interventions in and around drinking establishments that target crowding, management practice, physical design, staff training, and access to late night transportation also show promise in reducing violence (Bellis and Hughes 2008; Graham and Homel 2008).
Although most evidence for the effectiveness of interventions in preventing violence comes from HICs, several success stories come from LMICs, including the reduced trading hours in Brazil (Duailibi and others 2007). Given that LMICs show some of the greatest increases in alcohol consumption, more outcome evaluations of strategies to address alcohol-related violence in these settings are urgently needed. Two areas that should be explored are the effectiveness of (1) minimum drinking-age laws and (2) efforts to regulate the marketing of alcohol. However, in many LMICs, a large proportion of alcohol consumed is produced at home. In such settings, establishing policies to regulate alcohol production and sale is an important prerequisite for effective prevention (WHO and Liverpool John Moores University 2006). As WHO Member States, all LMICs are committed to implementing the global plan of action on alcohol and health (WHO 2010). That plan includes the interventions described.
Reducing Access to Lethal Means
Evidence from North America is the primary basis of two systematic reviews and one meta-analysis that summarize the effects of various strategies to prevent firearm-related violence. One systematic review (Hahn and others 2005) concluded that the evidence is insufficient to determine whether firearm laws have any effect on violence. Such laws include bans on specified firearms or ammunition, restrictions on the acquisition of firearms, waiting periods for acquisition, firearms registration, licensing of owners, “shall issue” carry laws that allow people who pass background checks to carry concealed weapons, child access prevention laws, and zero tolerance laws for firearms in schools. Another systematic review (Koper and Mayo-Wilson 2009) found that directed police patrols focusing on illegal gun carrying can prevent gun crimes (including murders, shootings, robberies in which guns are used, and armed assaults). One meta-analysis (Makarios and Pratt 2012) suggests that bans on the sale of firearms had small effects, and law enforcement strategies had moderate effects in reducing gun violence.
More recent evidence suggests that the use of street outreach workers to mediate conflicts and provide social support, such as job referrals and access to social services in the U.S. context, may be effective in reducing youth homicides and firearm offenses (Webster and others 2012). In addition, studies from Brazil and South Africa have found that stricter licensing and reduced circulation of firearms accounted for significant decreases in firearm-related injuries (Marinho de Souza and others 2007; Matzopoulos, Thompson, and Myers 2014). These reports therefore suggest, from a limited evidence base, that some strategies addressing access to firearms show promise, but additional research is needed.
Public health can make a critical contribution to preventing firearm injuries and deaths by collecting data and evidence. A range of strategies exists for reducing firearm-related violence, but further research and evidence are needed to assess their effectiveness (IOM and NRC 2013). Strategies identified by the Institute of Medicine (IOM) and others as being in particular need of additional research include the following:
-
Increasing efforts to control access to firearms by individuals at risk of harming themselves or others (for example, the safe storage of guns, waiting periods, and background checks)
-
Changing how firearms are used (for example, where firearms may be carried and provision of safety education)
-
Reducing the lethality of guns (for example, designing firearms to make them safer and addressing magazine size).
-
Evaluating strategies to reduce the use of military firearms in the aftermath of war or conflict, including strategies to disarm former combatants, disband armed groups, and reintegrate former combatants into civilian society.
Sound data and evidence on firearm injuries are needed to determine what programs and policies actually work in preventing these injuries while preserving the rights of legitimate gun owners.
Promoting Gender Equality to Prevent Violence against Women
Several outcome evaluation studies demonstrate the effectiveness of multisector interventions to prevent violence against women by promoting gender equality. The Intervention with Microfinance and Gender Equity in South Africa, which combines microloans and gender equity training, reduced rates of self-reported violence by more than 50 percent (Pronyk and others 2006). The Stepping Stones program implemented in Asia and Sub-Saharan Africa is a life skills training program that addresses gender-based violence, relationship skills, assertiveness training, and communication about HIV/AIDS and has shown promising results (Jewkes and others 2008; Paine and others 2002). The popularity of microfinance and conditional cash transfer programs in LMICs, into which violence prevention objectives could be integrated, further underscores their applicability.
Changing Cultural and Societal Norms That Support Violence
Interventions that challenge cultural and social norms supporting violence are widely used, and their relatively low cost makes them a popular option. Such interventions are often restricted to standalone mass-media campaigns that are intended to raise awareness about the harmful effects of violence, thereby reducing the likelihood of future acts of violence. No evidence shows that such campaigns are effective; however, some evidence suggests that programs combining awareness-raising efforts with other mechanisms to change norms (for example, social development and life skills training and legislation) are effective. In South Africa, the Soul City initiative used television (through a soap opera series), radio, and nationally distributed information booklets to raise awareness of new IPV laws. The intervention increased the proportion of people who saw such violence as unacceptable (Usdin and others 2005).
Implementing Victim Identification, Care, and Support Programs
Interventions to identify victims of interpersonal violence and to provide effective care and support are critical for protecting health and breaking cycles of violence from one generation to the next. Evidence of effectiveness is emerging in several areas:
-
Screening tools to identify victims of IPV and refer them to appropriate services (Ramsay and others 2002)
-
Psychosocial interventions, such as trauma-focused cognitive behavioral therapy, to reduce mental health problems associated with violence (Bass and others 2013; Kornør and others 2008)
-
Protection orders, which prohibit perpetrators of IPV from contacting victims (Holt and others 2003), to reduce repeat victimization.
Several trials have shown that advocacy support programs—which offer services such as counseling, safety planning, and referral—increase victims’ safety behaviors and reduce the risk of further harm (McFarlane and others 2006).
Policies and Programs to Address the Social Determinants of Violence
Violence is strongly associated with social determinants, such as employment, income equity, rapid social change, and access to education. The expectation that policies and programs can prevent violence by addressing social determinants derives from ecological studies that use cross-sectional and time-series methods to document associations between social determinants and violence. Comprehensive violence prevention strategies should do more than just address the risk factors targeted by the specific programs; such strategies should be integrated with policies directed at the inequities that fuel violence. This integration is particularly important in LMICs, where daily living conditions can undermine the opportunities for positive early child development. For example, the context can include economic and social policies that exacerbate gaps between rich and poor and between men and women.
Economic Evaluation of Interventions
Economic evaluation provides a way to compare gains resulting from an intervention, which has its own costs and risks. Given the high prevalence of interpersonal violence and its direct and indirect costs, identifying effective, low-cost interventions to reduce violence is an urgent priority. However, the same challenges that complicate measuring the costs of violence also complicate measuring the benefits associated with its prevention (Barnett 1993; WHO 2004). Despite widely varying methodologies, most studies show that behavioral, legal, and regulatory interventions are cost-effective (WHO 2004). Evidence addressing specific types of violence, largely from HICs, has identified a variety of cost-effective interventions to prevent child maltreatment, IPV, and youth violence (table 5.6). Despite the disproportionate effects of violence in LMICs, economic evaluations of interventions are rare; therefore, systematic research to measure the economic benefits of violence prevention efforts in LMICs would fill a critical gap.
Implementation of Prevention Strategies
The gap between the science and the practice of violence prevention is growing. Although numerous effective programs, policies, and innovations have been identified, they are unlikely to have a substantial public health impact unless they are widely disseminated, implemented with quality and scale, and sustained over the long term (Rhoades, Bumbarger, and Moore 2012). Moreover, the benefits of their implementation must also be monitored. The infrastructure needed to support the dissemination, scaling up, and sustenance of effective programs and policies is slowly emerging.
Given the rapid expansion of and increasing demand for evidence-based violence prevention innovations, especially in LMICs, building an infrastructure that can more effectively move innovations from research to action is increasingly important. That infrastructure requires attention to three interrelated sets of functions and activities that should be coordinated across global, country, and local levels: prevention synthesis and translation, prevention support, and prevention delivery (Wandersman and others 2008).
Prevention Synthesis and Translation
The greater the extent to which innovations for violence prevention are accessible (both from informational and financial perspectives), user-friendly, and clearly communicated, the more likely it is that effective approaches will be successfully disseminated and implemented (Clancy and Cronin 2005). The seven-part series on Violence Prevention: The Evidence is an example of an effort to synthesize and translate the scientific evidence into easily understandable and accessible briefing documents that demonstrate the effectiveness of interventions to prevent interpersonal and self-directed violence (Liverpool John Moores University 2013; WHO 2009).
Prevention Support
Synthesizing and translating information about violence prevention innovations, although important, are likely to be insufficient to change prevention practices. Countries, districts, and communities seeking to apply violence prevention innovations need the capacity to be successful in scaling up effective programs with fidelity (Wandersman and others 2008). A growing body of research suggests that providing support in the form of specialized training, monitoring of fidelity, technical assistance, and coaching, along with improving the skills and motivation of implementing organizations, increases the use and successful implementation of innovations (Fixsen and other 2005; Mihalic and Irwin 2003; Wandersman and others 2008).
An example of a well-functioning prevention support system in the United States is the state of Pennsylvania’s Evidence-Based Prevention and Intervention Support Center (EPISCenter) at the University of Pennsylvania (Rhoades, Bumbarger, and Moore 2012). The EPISCenter uses flexible, targeted, and research-based technical assistance to develop the capacity of communities to support the implementation of evidence-based violence prevention programs.
Prevention Delivery
The successful implementation of evidence-based innovations requires that they be carried out and sustained in organizational settings (Wandersman and others 2008). Organizations’ capacities to deliver the violence prevention innovations include maintaining a well-functioning organization; recruiting and maintaining well-trained staff members; developing community support; working with other organizations; and improving skills in selecting, implementing, and sustaining an innovation over time (Mihalic and Irwin 2003; Wandersman and others 2008). The Parent Centre in South Africa and Raising Voices in Uganda are two examples of organizations in LMICs that are seeking to sustain the implementation of interventions to prevent violence against women and children (Butchart and Hendricks 2000; The Parent Centre 2013; Raising Voices 2013).
Conclusions
The primary rationale for addressing interpersonal violence as a public health problem has been its role in causing physical injury and homicide. Evidence has shown that interpersonal violence also plays an important role in the etiology of mental illness, chronic disease, and even infectious diseases such as HIV/AIDS. Unfortunately, such wide-ranging effects remain largely invisible to public health leaders, policy makers, and the public. Violence is often hidden, victims rarely come into contact with official or service agencies, and many of the health and social consequences are not evident until years after exposure. Greater awareness of these impacts is now leading to actions that can reduce the enormous health and social burden of violence.
Many LMICs face daunting challenges, including the HIV/AIDS epidemic, ongoing wars and conflicts, cardiovascular and other chronic diseases, suicide, and traffic injuries. Given the effects of violence on these outcomes, preventing interpersonal violence can become a powerful lever that, if successfully engaged, will allow LMICs to more effectively address a broad range of challenges.
The study of violence crosses many domains, and collaboration across different government sectors and across different disciplines and professions is critical, both to fully understand the problem and to effectively prevent it. Violence affects almost every government sector, including justice and law enforcement, social services, protection of women and children, education, transportation, finance, health care and public health, labor, tourism, foreign affairs, interior affairs, commerce, and tourism. The disciplines that have important contributions to make include law, psychology, sociology, social work, medicine and almost every medical specialty, anthropology, engineering, business, architecture and design, and urban planning. Given this influence, the involvement of foundations, multilateral agencies, and corporations in programs to prevent violence is also expanding.
Progress in preventing interpersonal violence is advancing rapidly, and clearly the global public health community’s increased understanding and capacity to prevent interpersonal violence will make a difference. The lessons learned during their brief experience with violence prevention efforts are consistent with the lessons from the community’s much longer experience with the prevention of infectious and chronic diseases. Violence can be prevented if citizens, their governments, and the global community start now, act wisely, and work together.
Note
-
Corresponding author: James A. Mercy, U.S. Centers for Disease Control and Prevention, Atlanta, Georgia, United States; vog.cdc@2maj.
-
Disclaimer: The findings and conclusions in this chapter are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the World Health Organization (WHO).
-
World Bank Income Classifications as of July 2014 are as follows, based on estimates of gross national income per capita for 2013:
-
Low-income countries (LICs) = US$1,045 or less
-
Middle-income countries (MICs) are subdivided:a) Lower-middle-income = US$1,046 to US$4,125b) Upper-middle-income (UMICs) = US$4,126 to US$12,745
-
High-income countries (HICs) = US$12,746 or more.
-
References
-
Anda R F, Butchart A, Felitti V J, Brown D W. 2010. “Building a Framework for Global Surveillance of the Public Health Implications of Adverse Childhood Experiences.” American Journal of Preventive Medicine 39 (1): 93–98. [PubMed: 20547282]
-
Andersson N, Cockcroft A, Shea B. 2008. “Gender-Based Violence and HIV: Relevance for HIV Prevention in Hyperendemic Countries of Southern Africa.” AIDS 22 (S4): S73–86. [PubMed: 19033757]
-
Baker-Henningham H, Scott S, Jones K, Walker S. 2012. “Reducing Child Conduct Problems and Promoting Social Skills in a Middle-Income Country: Cluster Randomised Controlled Trial.” British Journal of Psychiatry 201 (2): 101–18. [PMC free article: PMC3409425] [PubMed: 22500015]
-
Barnett W S. 1993. “Economic Evaluation of Home Visiting Programs.” The Future of Children 3 (3): 93–112.
-
Bass J K, Annan J, McIvor S, Murray D, Kaysen S Griffiths., others. 2013. “Controlled Trial of Psychotherapy for Congolese Survivors of Sexual Violence.” New England Journal of Medicine 368 (23): 2182–91. [PubMed: 23738545]
-
Beaman V, Annest J L, Mercy J A, Kresnow M, Pollock D A. 2000. “Lethality of Firearm-Related Injuries in the United States Population.” Annals of Emergency Medicine 35 (3): 258–66. [PubMed: 10692193]
-
Bellis M A, Hughes K. 2008. “Comprehensive Strategies to Prevent Alcohol-Related Violence.” In Institute for the Prevention of Crime Review Volume 2: Towards More Comprehensive Approaches to Prevention and Safety, edited by Hastings R, Bania M, editors. 137–68. Ottawa: ON: Institute for Prevention of Crime.
-
Bellis M A, Hughes K, Perkins C, Bennett A. 2012. Protecting People, Promoting Health: A Public Health Approach to Violence Prevention for England. Liverpool, U.K.: Department of Health and National Health Service.
-
Bilukha O, Hahn R A, Crosby A, Fullilove M T, Liberman A., others. 2005. “The Effectiveness of Early Childhood Home Visitation in Preventing Violence: A Systematic Review.” American Journal of Preventive Medicine 28 (2): S11–39. [PubMed: 15698746]
-
Borwankar R, Diallo R, Sommerfelt A E. 2008. Gender-Based Violence in Sub-Saharan Africa: A Review of Demographic and Health Survey Findings and Their Use in National Planning. Washington, DC: United States Agency for International Development.
-
Bott S, Guedes A, Goodwin M, Mendoza J A. 2012. Violence against Women in Latin America and the Caribbean: A Comparative Analysis of Population-Based Data from 12 Countries. Washington, DC: Pan American Health Organization.
-
Buchanan C., ed. 2013. Gun Violence, Disability and Recovery. Sydney: Surviving Gun Violence Project.
-
Butchart A, Brown D, Khanh-Huynh A, Corso P, Florquin N., others. 2008. Manual for Estimating the Economic Costs of Injuries Due to Interpersonal and Self-Directed Violence. Geneva: World Health Organization.
-
Butchart A, Engstrom K. 2002. “Sex- and Age-Specific Effects of Economic Development and Inequality on Homicide Rates in 0 to 24 Year Olds: A Cross-Sectional Analysis.” Bulletin of the World Health Organization 80 (October): 797–805. [PMC free article: PMC2567653] [PubMed: 12471400]
-
Butchart A, Hendricks G. 2000. “The Parent Centre.” In Behind the Mask: Getting to Grips with Crime and Violence in South Africa, edited by Emmett T, Butchart A. 147–76. Pretoria: Human Sciences Research Council.
-
Buvinic M, Morrison A. R, Shifter M. 1999. “Violence in the Americas: A Framework for Action.” In Too Close to Home: Domestic Violence in the Americas, edited by Morrison A. R, Biehl M. L, editors. 3–34. New York: Inter-American Development Bank.
-
Caldera D L, Burrell K, Rodriguez S S, Crowne C Rohde. others. 2007. “Impact of a Statewide Home Visiting Program on Parenting and on Child Health and Development.” Child Abuse and Neglect 31 (8): 829–52. [PubMed: 17822765]
-
Capaldi D M, Knoble N B, Shortt J W, Kim H K. 2012. “A Systematic Review of Risk Factors for Intimate Partner Violence.” Partner Abuse 3 (2): 231–80. [PMC free article: PMC3384540] [PubMed: 22754606]
-
CDC (Centers for Disease Control and Prevention). 2003. Costs of Intimate Partner Violence against Women in the United States. Atlanta: National Center for Injury Prevention and Control.
-
CDC, INURED (Interuniversity Institute for Research and Development), and the Comité de Coordination. 2014. Violence against Children in Haiti: Findings from a National Survey, 2012. Port-au-Prince, Haiti: Centers for Disease Control and Prevention.
-
Chanley S A, Chanley J J, Campbell H E. 2001. “Providing Refuge: The Value of Domestic Violence Shelter Services.” American Review of Public Administration 31 (4): 393–413.
-
Clancy C M, Cronin K. 2005. “Evidence-Based Decision Making: Global Evidence, Local Decisions.” Health Affairs 24 (1): 151–62. [PubMed: 15647226]
-
Cohen A B. 2007. “Sobering Up: The Impact of the 1985–1988 Russian Anti-Alcohol Campaign on Child Health.” Unpublished paper, Tufts University, Boston, MA.
-
Cooper C, Selwood A, Livingston G. 2008. “The Prevalence of Elder Abuse and Neglect: A Systematic Review.” Age and Aging 37 (2): 151–60. [PubMed: 18349012]
-
Dahlberg L L, Krug E G. 2002. “Violence: A Global Public Health Problem.” In World Report on Violence and Health, edited by Krug E G, Dahlberg L L, Mercy J A, Zwi A B, Lozano R, editors. 1–21. Geneva: World Health Organization.
-
Danese A, McEwen B. 2012. “Adverse Childhood Experiences, Allostasis, Allostatic Load, and Age-Related Disease.” Physiology and Behavior 106 (1): 29–39. [PubMed: 21888923]
-
Day T., 1995. “The Health Related Costs of Violence against Women: The Tip of the Iceberg.” Centre for Research on Violence against Women and Children Publication Series, University of Western Ontario, London, Ontario.
-
Devries K, Watts C, Yoshihama M, Kiss L, Schraiber L B., others. 2011. “Violence against Women Is Strongly Associated with Suicide Attempts: Evidence from the WHO Multi-Country Study on Women’s Health and Domestic Violence against Women.” Social Science and Medicine 73 (1): 79–86. [PubMed: 21676510]
-
Dinh-Zarr T B, Goss C, Heitman E, Roberts E, DiGuiseppi C. 2004. “Interventions for Preventing Injuries in Problem Drinkers.” Cochrane Database of Systematic Reviews 3 (3): CD001857. [PMC free article: PMC7025439] [PubMed: 15266456]
-
Duailibi S, Ponicki W, Grube J, Pinsky I, Laranjeira R, Raw M. 2007. “The Effect of Restricting Opening Hours on Alcohol-Related Violence.” American Journal of Public Health 97 (12): 2276–80. [PMC free article: PMC2089093] [PubMed: 17971559]
-
Durlak J A, Weissberg R P, Pachan M. 2010. “A Meta-Analysis of After-School Programs That Seek to Promote Personal and Social Skills in Children and Adolescents.” American Journal of Community Psychology 45 (3–4):294–309. [PubMed: 20300825]
-
Eisenberg N, Zhou Q, Spinrad T L, Valiente C, Fabes R A. others. 2005. “Relations among Positive Parenting, Children’s Effortful Control, and Externalizing Problems: A Three-Wave Longitudinal Study.” Child Development 76 (5): 1055–71. [PMC free article: PMC1351058] [PubMed: 16150002]
-
Fang X, Brown D S, Florence C S, Mercy J A. 2012. “The Economic Burden of Child Maltreatment in the United States and Implications for Prevention.” Child Abuse and Neglect 36 (2): 156–65. [PMC free article: PMC3776454] [PubMed: 22300910]
-
Fanslow J, Coggan C, Miller B, Norton R. 1997. “The Economic Cost of Homicide in New Zealand.” Social Science and Medicine 45 (7): 973–97. [PubMed: 9257390]
-
Fisher J, Mello M Cabral de, Patel V, Rahman A, Tran T., others. 2012. “Prevalence and Determinants of Common Perinatal Mental Disorders in Women in Low- and Lower-Middle-Income Countries: A Systematic Review.” Bulletin of the World Health Organization 90 (2): 139–49. [PMC free article: PMC3302553] [PubMed: 22423165]
-
Fixsen D L, Naoom S F, Blase K A, Friedman R M, Wallace F. 2005. Implementation Research: A Synthesis of the Literature. Tampa, FL: University of South Florida, Louis de la Parte Florida Mental Health Institute, The National Implementation Research Network.
-
Florence C, Shepherd J, Brennan I, Simon T R. 2013. “An Economic Evaluation of Anonymised Information Sharing in a Partnership between Health Services, Police and Local Government for Preventing Violence-Related Injury.” Injury Prevention 20 (2): 108–14. doi:10.1136/injuryprev-2012-040622. [PMC free article: PMC5779858] [PubMed: 24048916]
-
Foshee V A, Bauman K E, Ennett S T, Suchindran C, Benefield T., others. 2005. “Assessing the Effects of the Dating Violence Prevention Program ‘Safe Dates’ Using Random Coefficient Regression Modeling.” Prevention Science 6 (3): 245–57. [PubMed: 16047088]
-
Foster E M, Jones D, the Conduct Problems Prevention Research Group. 2006. “Can a Costly Intervention Be Cost Effective? An Analysis of Violence Prevention.” Archives of General Psychiatry 63 (11): 1284–91. [PMC free article: PMC2753445] [PubMed: 17088509]
-
Giancola P., 2000. “Executive Functioning: A Conceptual Framework for Alcohol-Related Aggression.” Experimental and Clinical Psychopharmacology 8 (4): 576–97. [PubMed: 11127429]
-
Gilbert R, Widom C S, Browne K, Fergusson D, Webb E, Janson S. 2009. “Burden and Consequences of Child Maltreatment in High-Income Countries.” The Lancet 373 (9657): 68–81. [PubMed: 19056114]
-
Gore F M, Bloem P J N, Patton G C, Ferguson J, Joseph V., and others. 2011. “Global Burden of Disease in Young People Aged 10–24 Years: A Systematic Analysis.” The Lancet 377 (9783): 2093–102. [PubMed: 21652063]
-
Graham K, Homel R. 2008. Raising the Bar: Preventing Aggression in and around Bars, Pubs and Clubs. Devon, U.K.: Willan Publishing.
-
Greenwood P W, Model K E, Rydell C P, Chiesa J. 1996. Diverting Children from a Life of Crime: Measuring Costs and Benefits. Santa Monica, CA: Rand.
-
Habetha S, Bleich S, Weidenhammer J, Fegert J M. 2012. “A Prevalence-Based Approach to Societal Costs Occurring in Consequence of Child Abuse and Neglect.” Child and Adolescent Psychiatry and Mental Health 6: 35. doi:10.1186/1753-2000-6-35. [PMC free article: PMC3540003] [PubMed: 23158382]
-
Hahn R A, Bilukha O, Crosby A, Fullilove M T, Liberman A., others. 2005. “Firearms Laws and the Reduction of Violence: A Systematic Review.” American Journal of Preventive Medicine 28 (2S1): 40–71. [PubMed: 15698747]
-
Hahn R A, Fuqua-Whitley D, Wethington H, Lowy J, Crosby A., others. 2007. “Effectiveness of Universal School-Based Programs to Prevent Violent and Aggressive Behavior: A Systematic Review.” American Journal of Preventive Medicine 33 (2S): S114–29. [PubMed: 17675013]
-
Hawkins J D, Catalano R F, Kosterman R, Abbott R, Hill K G. 1999. “Preventing Adolescent Health-Risk Behaviors by Strengthening Protection during Childhood.” Archive of Pediatrics and Adolescent Medicine 153 (3): 226–34. [PubMed: 10086398]
-
Heim C, Binder E B. 2012. “Current Research Trends in Early Life Stress and Depression: Review of Human Studies on Sensitive Periods, Gene-Environment Interactions, and Epigenetics.” Experimental Neurology 233 (1): 102–11. [PubMed: 22101006]
-
Hillis S D, Anda R F, Dube S R, Felitti V J, Marchbanks P A, Marks J S. 2004. “The Association between Adverse Childhood Experiences and Adolescent Pregnancy, Long-Term Psychosocial Outcomes, and Fetal Death.” Pediatrics 113 (2): 320–27. [PubMed: 14754944]
-
Hillis S D, Anda R F, Dube S R, Felitti V J, Marchbanks P A., others. 2010. “The Protective Effect of Family Strengths in Childhood against Adolescent Pregnancy and Its Long-Term Psychosocial Consequences.” Permanente Journal 14 (3): 18–27. [PMC free article: PMC2937841] [PubMed: 20844701]
-
Holt V L, Kernic M A, Wolf M E, Rivara F P. 2003. “Do Protection Orders Affect the Likelihood of Future Partner Violence and Injury?” American Journal of Preventive Medicine 24 (1): 16–21. [PubMed: 12554019]
-
Hughes K, Bellis M A, Jones L, Wood S, Bates G., others. 2012. “Prevalence and Risk of Violence against Adults with Disabilities: A Systematic Review and Meta-Analysis of Observational Studies.” The Lancet 80 (9845): 899–907. doi:10.1016/S0410-6736(11)61851-5. [PubMed: 22795511]
-
ICRW (International Center for Research on Women). 2009. “Intimate Partner Violence: High Costs to Households and Communities.” Policy Brief, ICRW, Washington, DC.
-
IOM (Institute of Medicine). 2013. Evaluation of PEPFAR. Washington, DC: National Academies Press. [PubMed: 24901201]
-
IOM and NRC (National Research Council). 2012. Social and Economic Costs of Violence. Washington, DC: National Academies Press.
-
IOM and NRC (National Research Council). 2013. Priorities for Research to Reduce the Threat of Firearm-Related Violence. Washington, DC: National Academies Press.
-
Ireland T, Smith C. 2009. “Living in Partner-Violent Families: Developmental Links to Antisocial Behavior and Relationship Violence.” Journal of Youth and Adolescence 38 (3): 323–39. [PubMed: 19636748]
-
Jan J, Ferrari G, Watts C H, Hargreaves J R, Kim J C., others. 2011. “Economic Evaluation of a Combined Microfinance and Gender Training Intervention for the Prevention of Intimate Partner Violence in Rural South Africa.” Health Policy and Planning 26 (5): 366–72. [PubMed: 20974751]
-
Jewkes R K. 2002. “Intimate Partner Violence: Causes and Prevention.” The Lancet 359 (9315): 1423–29. [PubMed: 11978358]
-
Jewkes R K, Nduna M, Levin J, Jama N, Dunkle K., others. 2008. “Impact of Stepping Stones on Incidence of HIV and HSV-2 and Sexual Behaviour in Rural South Africa: Cluster Randomised Controlled Trial.” British Medical Journal 337: a506. doi:10.1136/bmj.a506. [PMC free article: PMC2505093] [PubMed: 18687720]
-
Kaminski J W, Valle L A, Filene J H, Boyle C L. 2008. “A Meta-Analytic Review of Components Associated with Parent Training Program Effectiveness.” Journal of Abnormal Child Psychology 36 (4): 567–89. [PubMed: 18205039]
-
Kessler R C, McLaughlin K A, Green J G, Gruber M J, Sampson N A. others. 2010. “Childhood Adversities and Adult Psychopathology in the WHO World Mental Health Surveys.” British Journal of Psychiatry 197 (5): 378–85. [PMC free article: PMC2966503] [PubMed: 21037215]
-
Kissin D M, Zapata L, Yorick R, Vinogradova E N, Volkova G V. others. 2007. “HIV Seroprevalence in Street Youth, St. Petersburg, Russia.” AIDS 21 (17): 2333–40. [PubMed: 18090282]
-
Klevens J, Martinez J W, Le B, Rojas C, Duque A., others. 2009. “Evaluation of Two Interventions to Reduce Aggressive and Antisocial Behavior in First and Second Graders in a Resource-Poor Setting.” International Journal of Educational Research 48 (5): 307–19.
-
Klosterman K C, Fals-Stewart W. 2006. “Intimate Partner Violence and Alcohol Use: Exploring the Role of Drinking in Partner Violence and Its Implications for Intervention.” Aggression and Violent Behavior 11 (6): 587–97.
-
Knerr W, Gardner F, Cluver L. 2013. “Improving Positive Parenting Skills and Reducing Harsh and Abusive Parenting in Low- and Middle-Income Countries: A Systematic Review.” Prevention Science 14 (4): 352–63. [PubMed: 23315023]
-
Koper C S, Mayo-Wilson E. 2009. “Police Strategies to Reduce Illegal Possession and Carrying of Firearms: Effects on Gun Crime.” Campbell Systematic Reviews 8 (11). doi:10.4073/csr.2012.11.
-
Kornør H, Winje D, Ekeberg Ø, Weisæth L, Kirkehei I., others. 2008. “Early Trauma-Focused Cognitive-Behavioural Therapy to Prevent Chronic Post-Traumatic Stress Disorder and Related Symptoms: A Systematic Review and Meta-Analysis.” BMC Psychiatry 8: 81. [PMC free article: PMC2559832] [PubMed: 18801204]
-
Krug E G, Dahlberg L I, Mercy J A, Zwi A B, Lozano R. eds. 2002. World Report on Violence and Health. Geneva: World Health Organization.
-
Kuklinski M R, Briney J S, Hawkins J D, Catalano R F. 2012. “Cost-Benefit Analysis of Communities That Care Outcomes at Eighth Grade.” Prevention Science 13 (2): 150–61. [PMC free article: PMC3305832] [PubMed: 22108900]
-
Lachs M S, Pillemer K. 2004. “Elder Abuse.” The Lancet 364 (9441): 1263–72. [PubMed: 15464188]
-
Lee S, Aos S, Drake E, Pennucci A, Miller M, Anderson L. 2012. “Return on Investment: Evidence-Based Options to Improve Statewide Outcomes, April 2012.” Document No. 12-04-1201, Washington State Institute for Public Policy, Olympia, WA.
-
Liverpool Johns Moores University. 2013. “Violence Prevention Evidence Base.” Database, Centre for Public Health, Liverpool John Moores University, Liverpool, U.K. http://www.preventviolence.info/EvidenceBase.
-
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K., others. 2012. “Global and Regional Mortality from 235 Causes of Death for 20 Age Groups in 1990 and 2010: A Systematic Analysis for the Global Burden of Disease Study 2010.” The Lancet 380 (9859): 2095–128. [PubMed: 23245604]
-
Machtinger E L, Haberer J E, Wilson T C, Weiss D S. 2012. “Recent Trauma Is Associated with Antiretroviral Failure and HIV Transmission Risk Behavior among HIV-Positive Women and Female-Identified Transgenders.” AIDS and Behavior 16 (8): 2160–70. Epub 2012/03/20. [PubMed: 22426597]
-
Machtinger E L, Wilson T C, Haberer J E, Weiss D S. 2012. “Psychological Trauma and PTSD in HIV-Positive Women: A Meta-Analysis.” AIDS and Behavior 16 (8): 2091–100. [PubMed: 22249954]
-
Makarios M D, Pratt C. 2012. “The Effectiveness of Policies and Programs That Attempt to Reduce Firearm Violence: A Meta-Analysis.” Crime and Delinquency 58 (2): 222–44.
-
Marinho de Souza M de F, Macinko J, Alencar A P, Malta D C, de O L, Neo Morais. 2007. “Reductions in Firearm-Related Mortality and Hospitalizations in Brazil after Gun Control.” Health Affairs 26 (2): 575–84. [PubMed: 17339689]
-
Markowitz S, Grossman M. 1998. “Alcohol Regulation and Domestic Violence towards Children.” Contemporary Economic Policy 16 (3): 309–20.
-
Markowitz S, Grossman M. 2000. “The Effects of Beer Taxes on Physical Child Abuse.” Journal of Health Economics 19 (2): 271–82. [PubMed: 10947580]
-
Mattson S N, Roesch S C, Glass L, Deweese B N, Coles C D. others. 2013. “Further Development of a Neurobehavioral Profile of Fetal Alcohol Spectrum Disorders.” Alcoholism: Clinical and Experimental Research 37 (3): 517–28. [PMC free article: PMC3524344] [PubMed: 22974253]
-
Matzopoulos R G, Thompson M L, Myers J E. 2014. “Firearm and Non-Firearm Homicide in Five South African Cities: A Retrospective Population-Based Study.” American Journal of Public Health 104 (3): 455–60. [PMC free article: PMC3953758] [PubMed: 24432917]
-
Mayhew P., 2003. “Counting the Costs of Crime in Australia.” Trends and Issues in Crime and Criminal Justice, no. 247. Australian Institute of Criminology, Canberra.
-
McFarlane J M, Groff J Y, O’Brien J A, Watson K. 2006. “Secondary Prevention of Intimate Partner Violence: A Randomized Controlled Trial.” Nursing Research 55 (1): 52–61. [PubMed: 16439929]
-
Mendonca R N, Alves J. G, Cabral J E Filho. 2002. “Hospital Costs Due to Violence against Children and Adolescents in Pernambuco State, Brazil, during 1999.” Cad Saude Publica 18 (6): 1577–81. [PubMed: 12488884]
-
Mihalic S, Irwin K. 2003. “Blueprints for Violence Prevention: From Research to Real World Settings: Factors Influencing the Successful Replication of Model Programs.” Youth Violence and Juvenile Justice 1: 307–29.
-
Mikton C, Butchart A. 2009. “Child Maltreatment Prevention: A Systematic Review of Reviews.” Bulletin of the World Health Organization 87 (5): 353–61. [PMC free article: PMC2678770] [PubMed: 19551253]
-
Miller M, Azrael D, Hemenway D. 2013. “Firearms and Violent Death in the United States.” In Reducing Gun Violence in America, edited by Webster D. W, Vernick J. S, editors. 1–20. Baltimore, MD: Johns Hopkins University Press.
-
Miller T R, Cohen M. A, Wiersema B. 1996. Victim Costs and Consequences: A New Look. National Institute of Justice Research Report, National Institute of Justice, United States Department of Justice, Washington, DC.
-
Miller T R, Fisher D A, Cohen M A. 2001. “Costs of Juvenile Violence: Policy Implications.” Pediatrics 107 (1): e3. [PubMed: 11134467]
-
Monteiro M., 2007. Alcohol and Public Health in the Americas: A Case for Action. Washington, DC: Pan American Health Organization.
-
Morrison A R, Orlando M B. 1999. “Social and Economic Costs of Domestic Violence: Chile and Nicaragua.” In Too Close to Home: Domestic Violence in the Americas, edited by Morrison A R, Orlando B E, editors. 51–80. New York: Inter-American Development Bank.
-
Nelson G, Westhues A, MacLeod J. 2003. “A Meta-Analysis of Longitudinal Research on Preschool Prevention Programs for Children.” Prevention and Treatment 6 (1): 31A. doi:10.1037/1522-3736.6.1.631a.
-
Nemtsov A V. 1998. “Alcohol-Related Harm and Alcohol Consumption in Moscow before, during and after a Major Anti-Alcohol Campaign.” Addiction 93 (10): 1501–10. [PubMed: 9926554]
-
Norman R, Spencer A, Eldridge S, Feder G. 2010. “Cost Effectiveness of a Programme to Detect and Provide Better Care for Female Victims of Intimate Partner Violence.” Journal of Health Services and Research Policy 15 (3): 143–49. [PubMed: 20308226]
-
Norman R E, Byambaa M, De R, Butchart A, Scott J., others. 2012. “The Long-Term Health Consequences of Child Physical Abuse, Emotional Abuse, and Neglect: A Systematic Review and Meta-Analysis.” PLoS Med 9 (11): e1001349. doi:10.1371/journal.pmed.1001349. [PMC free article: PMC3507962] [PubMed: 23209385]
-
Norton R, Kobusingye O. 2013. “Injuries.” New England Journal of Medicine 368 (18): 1723–30. [PubMed: 23635052]
-
Olds D, Henderson C R, Cole R, Eckenrode J, Kitzman H., others. 1998. “Long-Term Effects of Nurse Home Visitation on Children’s Criminal and Antisocial Behavior: 15-year Follow-Up of a Randomized Controlled Trial.” Journal of the American Medical Association 280 (14): 1238–44. [PubMed: 9786373]
-
Paine K, Hart G, Jawo M, Ceesay S, Jallow M., others. 2002. “Before We Were Sleeping, Now We Are Awake: Preliminary Evaluation of the Stepping Stones Sexual Health Programme in The Gambia.” African Journal of AIDS Research 1 (1): 41–52. [PubMed: 25871708]
-
The Parent Centre. 2013. “The Parent Centre: Helping Children through Parents.” http://www.theparentcentre.org.za/.
-
Pinheiro P S. 2006. World Report on Violence against Children. Geneva: United Nations.
-
Pronyk P M, Hargreaves J R, Kim J C, Morison L A, Phetla G., others. 2006. “Effect of a Structural Intervention for the Prevention of Intimate-Partner Violence and HIV in Rural South Africa: A Cluster Randomised Trial.” The Lancet 368 (9551): 1973–83. [PubMed: 17141704]
-
Raising Voices. 2013. “Raising Voices: Preventing Violence against Women and Children.” http://raisingvoices.org/about.
-
Ramsay J, Richardson J, Carter Y H, Davidson, Feder G. 2002. “Should Health Professionals Screen Women for Domestic Violence? Systematic Review.” British Medical Journal 325 (7359): 314. [PMC free article: PMC117773] [PubMed: 12169509]
-
Reed R, Fazel M, Jones L, Panter-Brick C, Stein A. 2012. “Mental Health of Displaced and Refugee Children Resettled in Low-Income and Middle-Income Countries: Risk and Protective Factors.” The Lancet 379 (9812): 250–65. [PubMed: 21835460]
-
Reza A, Mercy J A, Krug E G. 2001. “The Epidemiology of Violent Deaths in the World.” Injury Prevention 7 (2): 104–11. [PMC free article: PMC1730718] [PubMed: 11428556]
-
Reza A, Breiding M J, Gulaid G, Mercy J A, Blanton C., others. 2009. “Sexual Violence and Its Health Consequences for Female Children in Swaziland: A Cluster Survey Study.” The Lancet 373 (9679): 1966–72. [PubMed: 19428100]
-
Rhoades B L, Bumbarger B K, Moore J E. 2012. “TheRole of a State-Level Prevention Support System in Promoting High-Quality Implementation and Sustainability of Evidence-Based Programs.” American Journal of Community Psychology 50 (3): 386–401. [PubMed: 22441729]
-
Robbins C L, Zapata L, Kissin D M, Shevchenko N, Yorick R., others. 2010. “Multicity HIV Seroprevalence in Street Youth, Ukraine.” International Journal of STDs and AIDS 21 (7): 489–96. [PubMed: 20852199]
-
Roldós M I, Corso P. 2013. “The Economic Burden of Intimate Partner Violence in Ecuador: Setting the Agenda for Future Research and Violence Prevention Policies.” Western Journal Emergency Medicine 14 (4): 347–53. [PMC free article: PMC3735382] [PubMed: 23930148]
-
Rosenberg M L, Butchart A, Mercy J, Narasimhan V, Waters H., others. 2006. “Interpersonal Violence.” In Disease Control Priorities in Developing Countries, 2nd ed., edited by Jamison D T, Breman J G, Measham A R, Alleyne R G, Claeson M, editors. , others, 755–70. Washington, DC: Oxford University Press and World Bank. [PubMed: 21250309]
-
Silverman J G, Decker M R, Cheng D M, Wirth K, Saggurti N., others. 2011. “Gender-Based Disparities in Infant and Child Mortality Based on Maternal Exposure to Spousal Violence: The Heavy Burden Borne by Indian Girls.” Archives of Pediatric and Adolescent Medicine 165 (1): 22–27. [PMC free article: PMC3940346] [PubMed: 21199976]
-
Silverman J G R, Michele M R, Decker L, Heather M S McCauley., and others. 2009. “Regional Assessment of Sex Trafficking and STI/HIV in Southeast Asia: Connections between Sexual Exploitation, Violence, and Sexual Risk.” United Nations Development Programme Regional Center, Colombo. http://www.undp.org/content/dam/undp/library/hivaids/English/SexTrafficking.pdf.
-
Smith K W, Landry S H, Swank P R. 2010. “The Influence of Early Patterns of Positive Parenting on Children’s Preschool Outcomes.” Early Education and Development 11 (2): 147–69.
-
Stöckl H, Devries K, Rotsein A, Abrahams N, Campbell J., others. 2013. “The Global Prevalence of Intimate Partner Homicide: A Systematic Review.” The Lancet 382 (9895): 859–65. [PubMed: 23791474]
-
Stoltenborgh M A, van M. H, Ijzendoorn E M, Euser M J Bakermans-Kranenburg. 2011. “Global Perspective on Child Sexual Abuse: Meta-Analysis of Prevalence around the World.” Child Maltreatment 16 (2): 79–101. [PubMed: 21511741]
-
Stoltenborgh M A, Bakermans-Kranenburg M J, Ijzendoorn M H van, Alink L R. 2013a. “Cultural-Geographical Differences in the Occurrence of Child Physical Abuse? A Meta-Analysis of Global Prevalence.” International Journal of Psychology 48 (2): 81–94. [PubMed: 23597008]
-
Stoltenborgh M A, Bakermans-Kranenburg M J, van M H Ijzendoorn. 2013b. “The Neglect of Child Neglect: A Meta-Analytic Review of the Prevalence of Neglect.” Social Psychiatry and Psychiatric Epidemiology 48 (3): 345–55. [PMC free article: PMC3568479] [PubMed: 22797133]
-
Temple J A, Reynolds A J. 2007. “Benefits and Costs of Investments in Pre-School Education: Evidence from the Child-Parent Centers and Related Programs.” Economics of Education Review 26 (1): 126–44.
-
Tharp A T, Degue S, Valle L A, Brookmeyer K A, Massetti G M. others. 2012. “A Systematic Qualitative Review of Risk and Protective Factors for Sexual Violence Perpetration.” Trauma, Violence, and Abuse 14 (2): 133–67. [PubMed: 23275472]
-
Thornberry T P, Knight K E, Lovegrove P J. 2012. “Does Maltreatment Beget Maltreatment? A Systematic Review of the Intergenerational Literature.” Trauma, Violence and Abuse 13 (3): 135–52. [PMC free article: PMC4035025] [PubMed: 22673145]
-
UN (United Nations). 2006. Secretary General’s In-Depth Study on All Forms of Violence against Women. New York: United Nations.
-
UN (United Nations). 2015. Transforming Our World: The 2030 Agenda for Sustainable Development; Resolution Adopted by the General Assembly. 70/1. New York: United Nations. http://www.un.org/ga/search/view_doc.asp?symbolA/RES/70/1〈{{#}}0061;E.
-
UNICEF (United Nations Children’s Fund). 2010. Child Disciplinary Practices at Home: Evidence from a Range of Low- and Middle-Income Countries. New York: UNICEF.
-
UNICEF, CDC (Centers for Disease Control and Prevention), and KNBS (Kenya National Bureau of Statistics). 2012. Violence against Children in Kenya: Findings from a 2010 National Survey. Nairobi: UNICEF Kenya Country Office.
-
UNICEF, CDC, and the Muhimbili University of Health and Allied Science. 2012. Violence against Children in Tanzania: Findings from a National Survey 2009. Dar es Salaam, Tanzania: UNICEF Tanzania.
-
Usdin S, Scheepers E, Goldstein S, Japhet G. 2005. “Achieving Social Change on Gender-Based Violence: A Report on the Impact Evaluation of Soul City’s Fourth Series.” Social Science and Medicine 61 (11): 2434–45. [PubMed: 16006028]
-
van der Merwe A, Dawes A, Ward C L. 2012. “The Development of Youth Violence: An Ecological Understanding.” In Youth Violence in South Africa: Sources and Solutions, edited by Ward C L, Merwe A van der, Dawes A, editors. . Cape Town, South Africa: UCT Press.
-
Walker S P, Chang S M, Vera-Hernandez M, Grantham-McGregor S. . 2011. “Early Childhood Stimulation Benefits Adult Competence and Reduces Violent Behavior.” Pediatrics 127 (5): 849–57. [PubMed: 21518715]
-
Wandersman A, Duffy J, Flaspohler P, Noonan R, Lubell K., others. 2008. “Bridging the Gap between Prevention Research and Practice: The Interactive Systems Framework for Dissemination and Implementation.” American Journal of Community Psychology 41 (3–4):171–81. [PubMed: 18302018]
-
Ward E, McCartney T, Brown D W, Grant A, Butchart A., others. 2009. “Results of an Exercise to Estimate the Costs of Interpersonal Violence in Jamaica.” West Indian Medical Journal 58 (5): 446–51. [PubMed: 20441064]
-
Webster D W, Whitehill J M, Vernick J S, Curriero F C. 2012. “Effects of Baltimore’s Safe Streets Program on Gun Violence: A Replication of Chicago’s CeaseFire Program.” Bulletin of the New York Academy of Medicine 90 (1): 27–40. [PMC free article: PMC3579298] [PubMed: 22696175]
-
WHO (World Health Organization). 2004. The Economic Dimensions of Interpersonal Violence, edited by Waters H, Hyder A, Rajkotia Y, Basu S, Rehwinkel J A, editors. others. Geneva: WHO. http://whqlibdoc.who.int/publications/2004/9241591609.pdf.
-
WHO (World Health Organization). 2006. “Youth Violence and Alcohol Fact Sheet” (accessed June 30, 2013). http://www.who.int/violence_injury_prevention/violence/world_report/factsheets/ft_youth.pdf.
-
WHO (World Health Organization). 2008. Preventing Violence and Reducing Its Impact: How Development Agencies Can Help. Geneva: WHO. [PubMed: 18676792]
-
WHO (World Health Organization). 2009. Violence Prevention: The Evidence, Overview. Geneva: WHO.
-
WHO (World Health Organization). 2010. Global Strategy to Reduce the Harmful Use of Alcohol. Geneva: WHO.
-
WHO (World Health Organization). 2013. Global and Regional Estimates of Violence against Women: Prevalence and Health Effects of Intimate Partner and Non-Partner Sexual Violence. Geneva: WHO.
-
WHO (World Health Organization). 2014. “Global Health Estimates Summary Tables: Deaths by Cause, Age and Sex, by WHO Region.” WHO, Geneva. http://www.who.int/healthinfo/global_burden_disease/en/.
-
WHO (World Health Organization) and Liverpool John Moores University. 2006. “Interpersonal Violence and Alcohol.” WHO Policy Briefing. Geneva: WHO. http://www.who.int/violence_injury_prevention/violence/world_report/factsheets/pb_violencealcohol.pdf.
-
Wolfe D A, Crooks C, Jaffe P, Chiodo D, Hughes R., others. 2009. “A School-Based Program to Prevent Adolescent Dating Violence: A Cluster Randomized Trial.” Archives of Pediatrics and Adolescent Medicine 163 (8): 692–99. [PubMed: 19652099]
-
Zapata L B, Kissin D M, Robbins C L, Finnerty E, Skipalska H., others. 2011. “Multi-City Assessment of Lifetime Pregnancy Involvement among Street Youth, Ukraine.” Journal of Urban Health 88 (4): 779–92. [PMC free article: PMC3157496] [PubMed: 21779933]
-
Zapata L B, Kissin D M, Bogoliubova O, Yorick R V, Kraft J M. others. 2013. “Orphaned and Abused Youth Are Vulnerable to Pregnancy and Suicide Risk.” Child Abuse and Neglect 37 (5): 310–19. [PMC free article: PMC4465590] [PubMed: 23290621]
-
Zhao J, Stockwell T, Martin G, Macdonald S, Vallance K., and others. 2013. “The Relationship between Minimum Alcohol Prices, Outlet Densities and Alcohol-Attributable Deaths in British Columbia, 2002–2009.” Addiction 108 (6): 1059–69. doi:10.1111/add.12139. [PubMed: 23398533]
-
ZIMSTAT (Zimbabwe National Statistics Agency), UNICEF (United Nations Children’s Fund), and CCORE (Collaborating Centre for Operational Research and Evaluation). 2012. National Baseline Survey on Life Experiences of Adolescents in Zimbabwe 2011. Preliminary Report, ZIMSTAT, Harare, Zimbabwe.
Figures
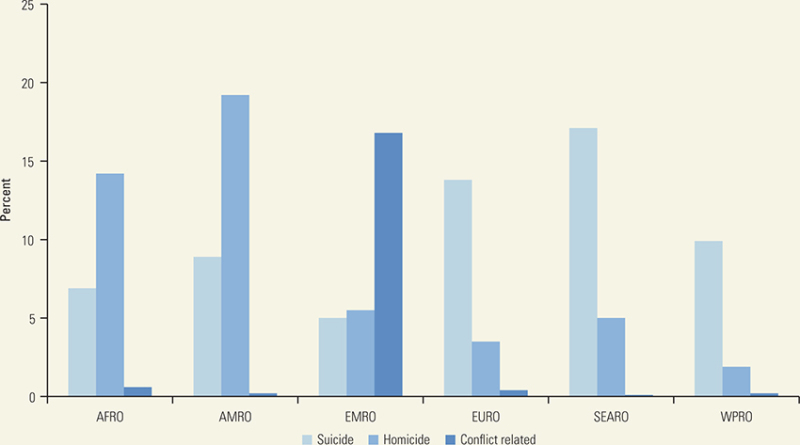
Figure 5.1
Homicide, Suicide, and Conflict-Related Fatality Rates, by Region, 2011
Note: AFRO = African Regional Office; AMRO = Americas Regional Office; EMRO = Eastern Mediterranean Regional Office; EURO = European Regional Office; SEARO = South-East Asia Regional Office; WPRO = Western Pacific Regional Office.
Tables
Table 5.1
Estimated Violence-Related Deaths, by Type and Income Level, 2011
| Category | Number | Rate per 100,000 peoplea | Proportion of total (percent) |
|---|---|---|---|
| Suicide | 803,900 | 11.4 | 56.3 |
| LMICs | 606,698 | 10.5 | 75.5 |
| HICs | 197,201 | 15.2 | 24.5 |
| Interpersonal | 504,587 | 7.1 | 35.3 |
| LMICs | 461,429 | 8.0 | 91.4 |
| HICs | 43,158 | 3.3 | 8.6 |
| Conflict related | 119,463 | 1.7 | 8.4 |
| LMICs | 117,131 | 2.0 | 98.0 |
| HICs | 2,332 | 0.2 | 2.0 |
| All types of violence | 1,427,949 | 20.2 | 100.0 |
| LMICs | 1,185,259 | 20.5 | 83.0 |
| HICs | 242,691 | 18.8 | 17.0 |
- a.
-
Age standardized.
-
Note: HIC = high-income country; LMIC = low- and middle-income country.
Table 5.2
Estimated Global Homicide and Suicide Rates, by Age and Gender, 2012
| Homicidesa | Suicidesa | |||
|---|---|---|---|---|
| Age | Males | Females | Males | Females |
| 0–4 years | 2.9 | 3.2 | 0.0 | 0.0 |
| 5–14 years | 2.0 | 1.6 | 1.2 | 1.2 |
| 15–29 years | 19.4 | 3.7 | 15.6 | 11.3 |
| 30–49 years | 15.4 | 2.8 | 17.6 | 7.8 |
| 50–59 years | 9.6 | 2.0 | 21.7 | 9.3 |
| 60–69 years | 6.8 | 2.2 | 24.6 | 13.1 |
| 70+ years | 6.4 | 3.5 | 43.2 | 20.8 |
| Total | 11.4 | 2.8 | 14.5 | 8.2 |
- a.
-
Per 100,000 people.
Table 5.3
Summary of Costs of Interpersonal Violence, by Types of Violence
| Study | Country | Costs included (time frame) | Discount rate | Total costs (per year) | Costs converted to 2013 U.S. dollars* | Violence-associated costs as percentage of national health expenditures | Violence-associated costs as percentage of GDP |
|---|---|---|---|---|---|---|---|
| Interpersonal violence in general | |||||||
| Miller, Cohen, and Wiersema 1996 | United States | Victim costs: medical and mental health care, victim services, productivity and quality of life losses (1993) (lifetime) | n.a. | US$358.0 billion for homicide, child abuse, sexual and other assault, and robbery (1993) | US$577.2 billion | n.a. | n.a. |
| Bellis and others 2012 | England and Wales | For homicide, wounding, assault, and sexual assault: criminal justice system, health and victim services, foregone output, and physical and emotional costs (lifetime) | n.a. | £29.9 billion (2008–09) | US$53.8 billion | n.a. | n.a. |
| Mayhew 2003 | Australia | For homicide, assault, and sexual assault: medical costs, lost wages, intangible costs such as pain, suffering, and reduced quality of life (annual) | n.a. | $A2.6 billion (2001) | US$1.8 billion | n.a. | n.a. |
| Fanslow and others 1997 | New Zealand | Lost earnings, legal fees, incarceration, and policing costs associated with homicide (annual) | n.a. | $NZ83.0 million, averaging $NZ1 million per homicide (1992) | US$74.9 million, averaging US$900 thousand per homicide | n.a. | n.a. |
| Buvinic, Morrison, and Shifter 1999 | Peru | For both interpersonal violence and collective violence: health impacts; private and public expenditures on police and security services; citizens’ willingness to pay to live without violence; and value of goods lost, ransoms, and bribes (annual) | n.a. | n.a. | n.a. | n.a. | 5.1 percentage of 1997 GDP |
| Buvinic, Morrison, and Shifter 1999 | Brazil | For both interpersonal violence and collective violence: health impacts; private and public expenditures on police and security services; citizens’ willingness to pay to live without violence; and value of goods lost, ransoms, and bribes (annual) | n.a. | n.a. | n.a. | n.a. | 10.5 percentage of 1997 GDP |
| Buvinic, Morrison, and Shifter 1999 | Venezuela, RB | For both interpersonal violence and collective violence: health impacts; private and public expenditures on police and security services; citizens’ willingness to pay to live without violence; and value of goods lost, ransoms, and bribes (annual) | n.a. | n.a. | n.a. | n.a. | 11.8 percentage of 1997 GDP |
| Buvinic, Morrison, and Shifter 1999 | Mexico | For both interpersonal violence and collective violence: health impacts; private and public expenditures on police and security services; citizens’ willingness to pay to live without violence; and value of goods lost, ransoms, and bribes (annual) | n.a. | n.a. | n.a. | n.a. | 12.3 percentage of 1997 GDP |
| Buvinic, Morrison, and Shifter 1999 | Colombia | For both interpersonal violence and collective violence: health impacts; private and public expenditures on police and security services; citizens’ willingness to pay to live without violence; and value of goods lost, ransoms, and bribes (annual) | n.a. | n.a. | n.a. | n.a. | 24.7 percentage of 1997 GDP |
| Buvinic, Morrison, and Shifter 1999 | El Salvador | For both interpersonal violence and collective violence: health impacts; private and public expenditures on police and security services; citizens’ willingness to pay to live without violence; and value of goods lost, ransoms, and bribes (annual) | n.a. | n.a. | n.a. | n.a. | 24.9 percentage of 1997 GDP |
| Butchart and others 2008 | Brazil | Lifetime medical and productivity losses associated with self-directed and interpersonal violence (lifetime) | 3 percent | R$16.1 billion (2004) | US$6.4 billion | 0.4 percent | 1.2 percentage of 2004 GDP |
| Butchart and others 2008 | Jamaica | Lifetime medical and productivity losses associated with self-directed and interpersonal violence (lifetime) | 3 percent | J$29.6 billion (2006) | US$530.0 million | 12.0 percent | 4.0 percentage of 2006 GDP |
| Butchart and others 2008 | Thailand | Lifetime medical and productivity losses associated with self-directed and interpersonal violence (lifetime) | 3 percent | B15.7 billion (2005) | US$453.3 million | 4.0 percent | 0.4 percentage of 2005 GDP |
| Child maltreatment | |||||||
| Fang and others 2012 | United States | Childhood health care, adult medical, lost productivity, child welfare, criminal justice, and special education costs (lifetime) | 3 percent |
|
US$132.5 billion | n.a. | n.a. |
|
|||||||
|
|||||||
| Habetha and others 2012 | Germany | Costs associated with health care, social, and educational services; foster care; productivity losses (lifetime) | n.a. | €11.1 billion (2008) | US$9.7 billion | n.a. | n.a. |
| Mendonca, Alves, and Cabral Filho 2002 | Recife, Brazil | Hospital costs (annual) | n.a. | n.a. | n.a. | Violence against children and adolescents accounted for 65.1 percent of hospital admissions and 77.9 percent of all hospital costs in the state of Pernambuco (1999) | n.a. |
| Intimate partner violence | |||||||
| CDC 2003 | United States | Medical and mental health care costs, lost productivity (annual) | n.a. | US$5.8 billion (1995) | US$8.9 billion | n.a. | n.a. |
| Day 1995 | Canada | Costs of health care, policing, legal fees, incarceration, lost earnings, and psychological trauma (lifetime) | n.a. | Can$1.2 billion (1992) | US$1.7 billion | n.a. | n.a. |
| Morrison and Orlando 1999 | Chile | Lost productive capacity of abused women (annual) | n.a. | Ch$1.6 billion (1996) | US$5.8 million | n.a. | 2.0 percentage of 1996 GDP |
| Morrison and Orlando 1999 | Nicaragua | Lost productive capacity of abused women (annual) | n.a. | C$29.5 million (1996) | US$5.2 million | n.a. | 1.6 percentage of 1996 GDP |
| International Center for Research on Women 2009 | Bangladesh | Costs of health care, justice, and lost productivity (annual) | n.a. | n.a. | n.a. | n.a. | 4.5 percentage of 2007 per capita gross national income |
| International Center for Research on Women 2009 | Morocco | Costs of health care, justice, and lost productivity (annual) | n.a. | n.a. | n.a. | n.a. | 22.0 percentage of 2007 per capita gross national income |
| International Center for Research on Women 2009 | Uganda | Costs of health care, justice, and lost productivity (annual) | n.a. | n.a. | n.a. | n.a. | 4.0 percentage of 2007 per capita gross national income |
| Roldós and Corso 2013 | Ecuador | Costs of medical and legal services, and productivity losses (annual) | n.a. | US$109.0 million (2012) | US$110.6 million | n.a. | n.a. |
| Youth violence | |||||||
| Miller, Fisher, and Cohen 2001 | Pennsylvania, United States | Total victim costs, including quality of life and productivity losses of juvenile violence (lifetime) | 2.5 percent | US$5.4 billion (1993) | US$8.7 billion | n.a. | n.a. |
Note: * Conversions to 2013 U.S. dollars using Department of Labor Consumer Price Index Inflation Calculator; GDP = gross domestic product; n.a. = not applicable.
Table 5.4
Risk for Perpetrating Violence
| Level of the ecological model | Risk factors |
|---|---|
| Individual |
|
| Household |
|
| Peer group |
|
| Community |
|
| Societal |
|
Table 5.5
Overview of Violence Prevention Strategies Showing Evidence for Effectiveness and Applicability in Low- and Middle-Income Countries
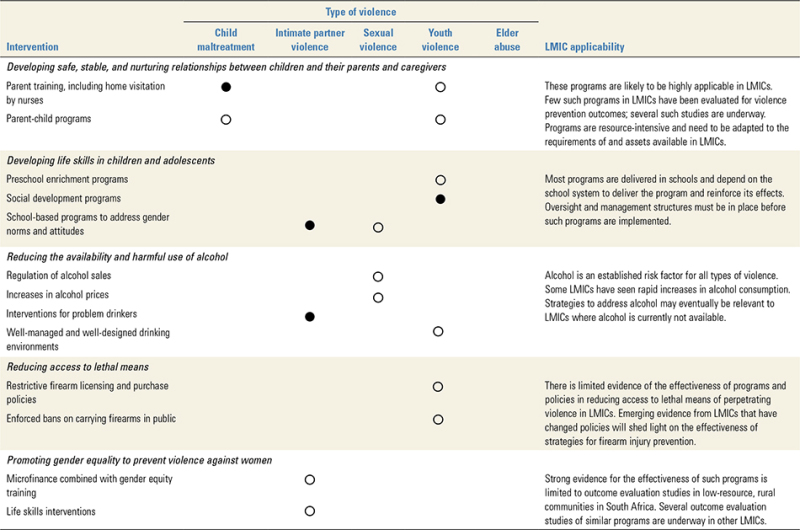
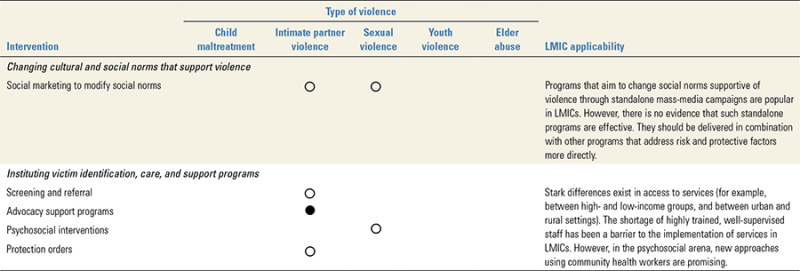
Note: LMICs = low- and middle-income countries;  = well supported by evidence (multiple randomized controlled trials with different populations);
= well supported by evidence (multiple randomized controlled trials with different populations);  = emerging evidence.
= emerging evidence.
Table 5.6
Summary of Economic Evaluations of Interventions to Prevent Interpersonal Violence, by Type of Violence
| Type of violence | Intervention type | Intervention details | Cost-effectiveness |
|---|---|---|---|
| Child maltreatment | Home visiting | Nurse-family partnerships provide home visiting for low-income mothers to improve prenatal health-related behaviors, provide more responsible and competent care of infants and toddlers, and improve parents’ economic self-sufficiency (Lee and others 2012). Location: United States |
Net benefit (in 2011 dollars) for each program participant was US$13,181 (US$13,617 in 2013 dollars); benefit-to-cost ratio was US$2.37 for every US$1.00 spent (US$2.46 in 2013 dollars). |
| Parent-child interaction therapy | Empirical treatment for conduct disorders is based on behavioral interventions to improve parent-child interaction (Lee and others 2012). Location: United States |
Net benefit (in 2011 dollars) for each program participant was US$5,617 (US$5,820 in 2013 dollars); benefit-to-cost ratio was US$4.62 for every $1.00 spent (US$4.79 in 2013 dollars). | |
| Educational and family support | The Child-Parent Center Program is a program for economically disadvantaged children and parents that provides a stable early learning environment and educational and support services for parents (Temple and Reynolds 2007). Location: Chicago, Illinois |
Range of benefit-to-cost ratio (in 2002 dollars) was US$5.98 (US$7.76 in 2013 dollars) to US$10.15 (US$13.18 in 2013 dollars) for every US$1.00 spent. | |
| Intimate partner violence (IPV) | Microfinance with gender and human immunodeficiency virus/acquired immune deficiency syndrome (HIV/AIDS) training | The Intervention with Microfinance for AIDS and Gender Equity (IMAGE) provides a combination of microfinance with gender and HIV/AIDS training for women to improve health, income, behavioral skills, communication, and norms (Jan and others 2011). Location: Rural South Africa |
Cost per disability-adjusted life year averted for the initial scale-up was US$2,307 (in 2004 dollars; US$2,852 in 2013 dollars). |
| Education for primary care providers | Training allows clinicians to increase their identification and referral of survivors of IPV (Norman and others 2010). Location: United Kingdom |
Incremental cost-effectiveness ratio was £2,450 per quality-adjusted life year (in 2005 pounds) ($4,228 in 2013 dollars). | |
| Shelters for victims | Shelters provide a safe haven for women and child victims of IPV, including support and safety planning (Chanley, Chanley, and Campbell 2001). Location: Arizona |
Net social benefit was US$3.4 million dollars (in 1999 dollars); minimum benefit-to-cost ratio was US$4.60 for every US$1.00 spent (US$6.45 in 2013 dollars). | |
| Youth violence | Anonymized information sharing between police and hospital emergency department | The Cardiff model provides information to direct targeted prevention measures. Youth were among those most likely to benefit (Florence and others 2013). Location: Cardiff, United Kingdom |
The cumulative social benefit-to-cost ratio was £82 (in 2003 pounds) for every £1.00 spent (US$163 in 2013 dollars). |
| Multicomponent, long-term school and family-based program | Fast Track, a program for at-risk children in grades 1–10, includes tutoring, parent support, child social-skills training, and home visits (Foster, Jones, and the Conduct Problems Prevention Research Group 2006). Location: Durham, North Carolina; Nashville, Tennessee; Seattle, Washington; and rural central Pennsylvania |
The intervention was not cost-effective at a threshold of US$50,000 willingness to pay (in 2004 dollars; US$61,817 in 2013 dollars) for an act of interpersonal violence. | |
| Mobilization of community stakeholders to implement evidence-based systems | Communities That Care (CTC) mobilizes stakeholders to collaborate on preventing adolescent substance use, delinquency, and interpersonal violence (Kuklinski and others 2012). Location: 24 communities in seven states |
Very cost beneficial in the United States; net present benefit of CTC was US$5,250 per youth (in 2004 dollars; US$6,491 in 2013 dollars), with a benefit-to-cost ratio of US$5.30 for every US$1.00 spent (US$6.55 in 2013 dollars). | |
| Educational incentives | Incentives included four years of cash and other incentives to induce disadvantaged high school students to graduate (Greenwood and others 1996), Location: California |
For every US$1.0 million (in 1993 dollars; $1.62 million in 2013 dollars), 258 serious crimes were prevented. | |
| Parent training and family therapy | The intervention included training for parents and therapy for families with young school-age children who have shown aggressive behavior (Greenwood and others 1996). Location: California |
For every US$1.0 million (in 1993 dollars; US$1.62 million in 2013 dollars), 157 serious crimes were prevented. | |
| Supervision | The intervention included monitoring and supervising high school–age youth who have exhibited delinquent behavior (Greenwood and others 1996). Location: California |
For every US$1.0 million (in 1993 dollars; US$1.62 million in 2013 dollars), 72 serious crimes were prevented. | |
| Home visiting and day care | The intervention included home visits by child care professionals from birth through the first two years of childhood, followed by four years of day care (Greenwood and others 1996). Location: California |
For every US$1.0 million (in 1993 dollars; US$1.62 million in 2013 dollars), 11 serious crimes were prevented. |

